פוסט זה זמין גם ב:
עברית
Written by Clay Smith
Spoon Feed
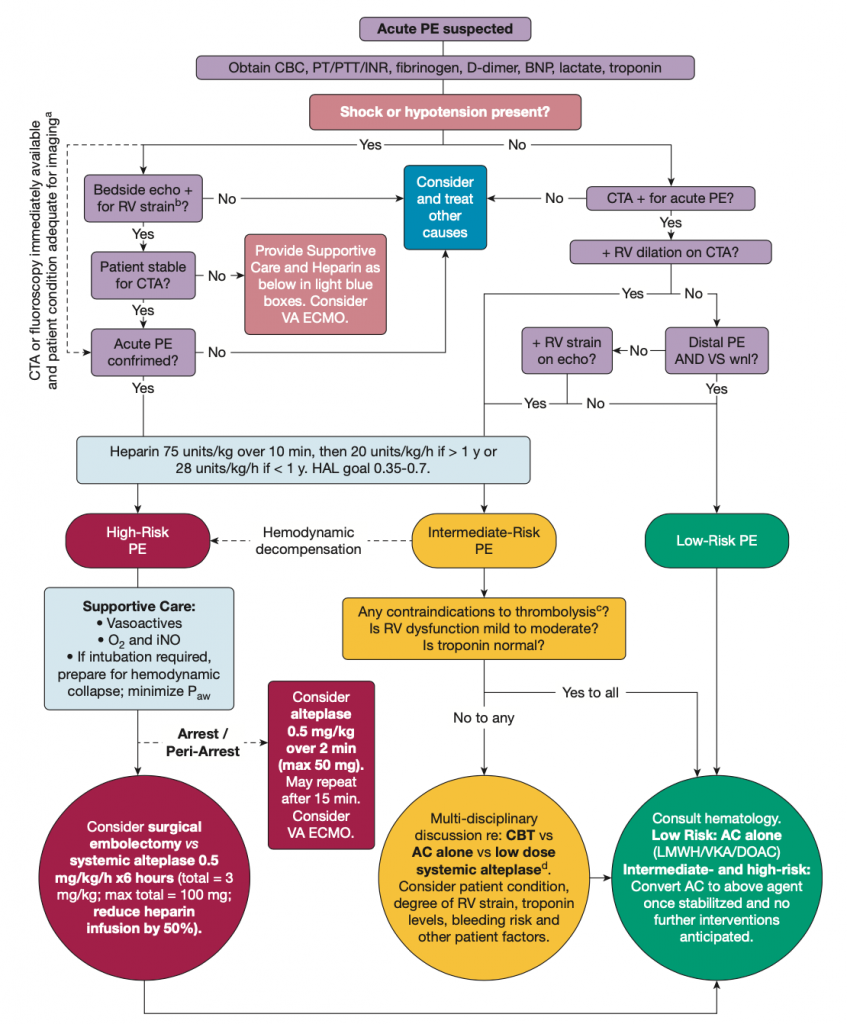
This is a spoon-feed version of the management of massive and submassive PE in children.
Why does this matter?
PE has become more common in children and rarely causes severe disease. Current pediatric guidelines mirror those of adults. This group of experts seeks to consider how things might need to be tailored for children. What are best management practices in children when managing massive or submassive PE in children?
PE in children – adult guidelines tailored for kids
Presentation
- Symptoms of PE may be more subtle in children, especially non-verbal children. Risk-stratification tools and labs, like Wells score and D-dimer, don’t perform as well in children.
- Watch for big PE risk factors in kids, such as estrogen use, cancer, obesity, central lines, and inherited thrombophilias.
- Though they cited this article, this review didn’t mention that the PERC rule performed well in a small, retrospective study of pediatric patients.
Definitions
- High-risk (aka massive) PE in children – This is defined similarly to adults, except the authors note that hypotension is often late or absent, and children may be normotensive yet have signs of poor perfusion and shock. A “compensated shock” presentation (think PALS) should also be considered massive PE. Hypotension should be defined using <5th percentile based on age-specific norms. PALS considers hypotension to be a SBP = 70 + 2(age), if age 1-10 years old.
- Intermediate-risk (aka submassive) PE in children – This is also defined similarly to adults: no hypotension or poor perfusion but with RV strain on imaging (CT or echo) and elevated troponin. I would also add elevated BNP.
Management
- High-risk: Primary reperfusion by thrombolysis or embolectomy is warranted. “Boston Children’s Hospital currently uses alteplase 0.5 mg/kg/h over 6 h for a total of 3 mg/kg with a maximum of 100 mg.” Surgical embolectomy is preferred in cases of tumor thrombus, such as Wilms, Ewings, or osteosarcoma, for example. Not much has been written on catheter-based therapy (CBT) in children. Epinephrine is recommended for hemodynamic support as needed in children over norepinephrine. Optimize oxygenation and hemodynamics as much as possible if placing on mechanical ventilation. Consider ECMO if unstable despite interventions. If high suspicion or confirmed PE is followed by arrest, intra-arrest tPA may be indicated. Authors recommend alteplase 0.5 mg/kg (maximum, 50 mg) over 2 min. Bleeding risk is greater in children with thrombolysis or anticoagulation.
- Intermediate-risk: In general, thrombolysis is not recommended in adults, and the same goes for children. However, authors recommend this be decided on a case by case basis, and if done, CBT is recommended.
This review is limited by the fact that the majority of PE literature is in adults, and most of the recommendations that are pediatric-specific are based on expert opinion. That said, I agree with their opinions and think they make a lot of sense.
Authors propose this algorithm.
Source
Acute Management of High-Risk and Intermediate-Risk Pulmonary Embolism in Children: A Review. Chest. 2022 Mar;161(3):791-802. doi: 10.1016/j.chest.2021.09.019. Epub 2021 Sep 26.





