Written by Clay Smith
Spoon Feed
Here are the clues from ECG, echo, and biomarkers that can help distinguish STEMI from pericarditis.
Why does this matter?
Chest pain may mean a lot of things – some dangerous, some not. Both STEMI and pericarditis lead to ST elevation. What are the clues to tell them apart?
STEMI vs pericarditis
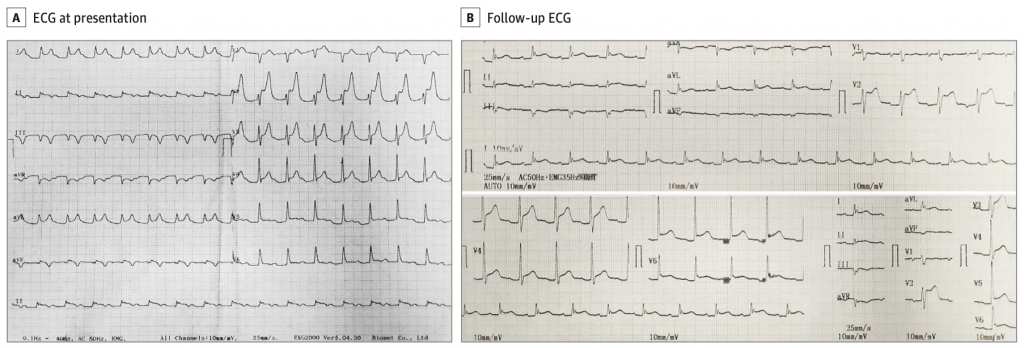
This was a case report of a 57 year old man with persistent chest pain, worse with cough, radiating to the back 8 hours after failed streptokinase therapy that was administered the day prior (time from lytic bolus to this episode of pain was 8 hours). He was mildly dyspneic, with otherwise normal vitals and a pericardial friction rub on exam.
There are 3 ways to distinguish STEMI from pericarditis: ECG, echo, and biomarkers (other).
ECG clues
- Usually pericarditis has diffuse concave ST elevation in the precordial and limb leads, with no reciprocal changes or Q waves and upright T waves. There is often diffuse PR depression, except in aVR, which has PR elevation and ST depression (so called ‘knuckle sign’).
- STEMI usually has convex ST elevation in an anatomic distribution, reciprocal changes, T wave inversion, and subsequent Q waves.
- Inferior STEMI may have sinus bradycardia or total AV block (TAVB), as the sinoatrial node, AV node, and his bundle are supplied by the RCA.
Echo
- Only 60% of pericarditis cases have pericardial effusion.
- Regional wall motion abnormalities can provide a major clue that STEMI is the culprit rather than pericarditis
Biomarkers (other)
- Elevated troponin also favors STEMI, though it could indicate perimyocarditis. Myocarditis may also have wall motion abnormalities and conduction system defects.
- Ultimately, as in this case report, cardiac angiography can help distinguish the two.
- Cardiac MRI can help, and endomyocardial biopsy definitively confirms perimyocarditis.
Conclusion: The patient had elevated troponin, inferior and posterior wall motion abnormalities and minimal pericardial effusion on echo, intermittent – worsening TAVB, and was found to have 99% occlusion of the RCA, which was stented.
Source
Diagnostic Dilemma of Pericarditis Concurrent With ST Elevation Myocardial Infarction. JAMA Intern Med. 2022 Mar 21. doi: 10.1001/jamainternmed.2022.0318. Online ahead of print.









