Podcast: Play in new window | Download
In this Part 1 or our two part podcast series on Red Flag Headaches we discuss a general approach, tips and tricks to assessing patients who present with headache followed by a deep dive into cervical artery dissections. With the help of Dr. Roy Baskind and Dr. Amit Shah we answers questions such as: what are the big 5 headache diagnoses that are not routinely picked up on plain CT or LP? Why are the symptoms of cervical artery dissection often fluctuating? Why do the symptoms of cervical artery dissection sometimes seem to not fit an anatomical distribution? What are the key clinical features that would trigger you to suspect cervical artery dissection? How do you decide which patients require a CT angiogram? What is the evidence for a causal relationship between chiropractic manipulation and cervical artery dissections? What is evidence for antiplatelet agents, anticoagulants and thrombolysis in the management of cervical artery dissection? Which patients with cervical artery dissection can be safely discharged from the ED and many more…
Podcast production, sound design & editing by Anton Helman
Written Summary and blog post by Humna Amjad, edited by Anton Helman Novebmer, 2021
Cite this podcast as: Helman, A. Shah, A. Baskind, B. Episode 161 Red Flag Headaches: General Approach and Cervical Artery Dissections. Emergency Medicine Cases. November, 2021. https://emergencymedicinecases.com/red-flag-headaches-cervical-artery-dissections. Accessed [date]
The big 5 causes of emergency headaches that are not routinely identified on plain CT or LP
Headaches are one the most common ED presentations. About 98% of these patients have a benign cause of their headache. Of the remaining 2%, 1% can be diagnosed with a CT head or LP, such as a subarachnoid hemorrhage or meningitis, however the final 1% causes of headaches cannot be ruled out on plain CT/LP alone. The big five commonly missed emergency causes of headaches that cannot routinely be ruled out on plain CT/LP include:
- Cervical artery dissection (carotid and vertebral)
- Cerebral venous thrombosis (CVT)
- Idiopathic Intracranial Hypertension (IIH)
- CO poisoning
- Giant cell arteritis
In this part 1 of our 2-part podcast on red flag headaches we focus on a general approach to headaches in the ED and cervical artery dissection – one of the big five causes of emergency headaches that does not show up routinely on plain CT, requiring a CT angiogram of the head and neck to confirm the diagnosis.
Some clinical pearls for headache assessment
- Headaches can arise from referred pain from the neck and neck pain can arise from referred pain from the head; include neck pathology in patients who present with headache and vice versa
- Clinical features that should trigger the consideration for a serious cause of headache include rapid onset of pain within minutes, repeat visits to ED for the same headache, exertional headache, different to previous headaches, focal neurologic findings, papilledema, immunocompromised state, loss of vision and abnormal vital signs
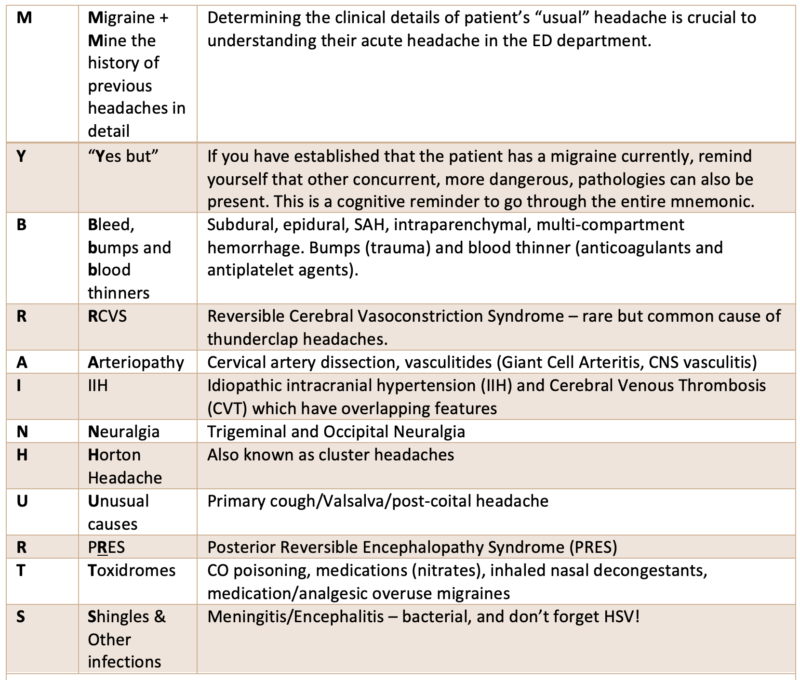
Dr. Baskind’s general approach to headache differential diagnosis: MY BRAIN HURTS
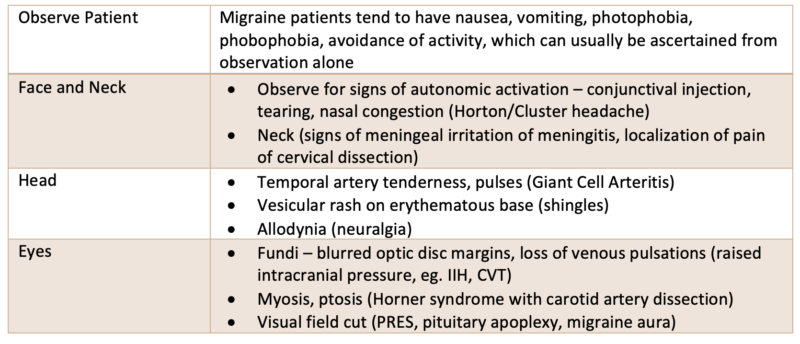
Dr. Baskind’s physical examination tips suggesting specific diagnoses for patients presenting with headache
Cervical artery dissection is often difficult to diagnose in the ED
Carotid and vertebral artery dissections cause up to 25% of strokes in young patients. They can occur spontaneously or following neck trauma, which may be minor in force. They are difficult to diagnose, especially on initial visit to the ED, because headache and/or neck pain may be their only symptom(s), stroke symptoms, which occur in a about 2/3 of patients, may be delayed by hours, days or even weeks, and neurologic deficits may be fluctuating, transient (may be completely resolved by the time they present to the ED), and often do not fit a typical stroke large vessel arterial distribution.
Pathophysiology of cervical artery dissection is important to help understand the clinical features
A tear occurs in the intimal lining of the artery which initiates a dissection along the length of the artery. This typically coincides with the acute head/face/neck pain that may be migratory. An intramural hematoma develops with subintimal dissections that lead to stenosis and may also cause complete occlusion. Thrombi may dislodge causing downstream occlusion and showering of emboli can flow to various locations causing a variety of neurologic symptoms that do not fit a typical large vessel occlusion distribution. In addition to the ischemic phenomena there may be concurrent stretching of vessel by the local clot/distension which can have local peripheral neurologic effects such as partial Horner’s Syndrome and cranial neuropathies.
Key risk factors for cervical artery dissection
- Any trauma (even minor) that may stretch or torque a cervical artery. Observational data suggests that up to 80% of cervical artery dissections are preceded by some form of blunt or penetrating trauma to head or neck. The trauma may be so benign that the patient does not remember it (i.e. vomiting, yoga, massage, shaving, swimming), however a causal relationship is difficult to prove for these minor mechanisms.
- Post-chiropractor manipulation: The absolute incidence of dissection following chiropractic manipulation is unknown. It is also unknown whether dissections diagnosed following chiropractic manipulation were caused by the neck manipulation or by a prior minor trauma causing the neck pain that brought them to the chiropractor in the first place.
- Connective tissue disorders (Marfan syndrome, Ehler-Danlos)
- Migraine – Observational studies suggest that patients with migraines are at 2x the risk for dissection (be cautious ascribing all symptoms to a migraine!)
- Infection: Recent infections, particularly respiratory infections, have been suggested to predispose patients to CAD
- Other risk factors include: OCP use, smoking, pregnancy/postpartum
Clinical features: local cervical artery dissection phenomena
- Pain (57-90% of patients): neck pain and headache are usually the most prominent features; may affect the jaw or face and may migrate between these areas; quality of pain is variable, may be constant, intermittent or fluctuating, and onset may be thunderclap (mimicking SAH) or gradual;
- Partial Horner’s Syndrome (25% of patients): due to local expansion (secondary to thrombus stretching the vessel) affecting the sympathetic fibres travelling along the internal carotid. Ptosis, miosis, but no anhidrosis (as fibres for sweat travel along the external carotid).
- Cranial neuropathies (12% of patients): due to compression; most commonly CN 12 and 9.
- Pulsatile tinnitus has been noted in 8% of patients
- Subarachnoid Hemorrhage: can be occur if the dissection extends intracranially.
Pearl: After a negative ED workup for SAH with plain CT +/- LP in a patient who presents with thunderclap headache, consider cervical artery dissection, as cervical artery dissection may present with thunderclap headache.
Difference in clinical presentation between carotid and vertebral artery dissections
It is important to note that in cervical artery dissections, ischemic symptoms tend to follow local symptoms by hours to a few days and may be transient or fluctuating, unilateral or bilateral, have a classic large vessel occlusion pattern or a variety of seemingly “non-anatomic” patterns.
Carotid artery dissection pain is typically located over the anterolateral aspect of the neck and may radiate to the jaw/face/head. Ischemic symptoms may include MCA/ACA circulation stroke syndromes, transient monocular blindness (amaurosis fugax) and retinal artery occlusion. Local effects include partial Horner’s Syndrome and cranial nerve 12 and 9 deficits. CNS deficits are typically contralateral to the dissection.
Vertebral artery dissection pain is typically unilateral, located in the postero-lateral neck and occiput and may lead to Wallenberg Syndrome (dysmetria, ataxia, ipsilateral hemiplegia and contralateral loss of pain and temperature sensation) and other posterior circulation stroke syndromes – i.e. vertigo, diplopia, visual field deficits. CNS deficits may be contralateral or bilateral.
Clinical Pearl: Migraines cause ipsilateral neurological symptoms. Carotid artery dissections cause contralateral symptoms whereas vertebral artery dissections can cause contralateral OR bilateral symptoms
ED management of cervical artery dissections
The management of cervical artery dissection is variable across institutions as there is mixed/unclear evidence. As with any patient with an acute stroke, blood pressure considerations, glucose control and airway management principles apply.
Selection of anti-thrombotic therapy
For extracranial dissection – either an antiplatelet agent or an anticoagulant (usually LMWH) is generally recommended and there is no clear agreement in the literature as to which one is optimal.
- The limited research evidence suggests that there is no difference in efficacy between antithrombotic agents for preventing ischemic strokes for extracranial dissections
- CADISS Trial: RCT of 250 patients: no difference in any outcomes between anticoagulants and antiplatelet agents at 12 month follow up
- TREAT-CAD Trial involved 194 patients: tested non-inferiority of aspirin compared to vitamin K antagonist. The composite endpoint (death, stroke, major hemorrhage) occurred more often in the aspirin group compared with the vitamin K antagonist group (23 versus 15 percent, absolute difference 8 percent, 95% CI -4 to 21 percent); while the difference was not statistically significant, aspirin failed to meet noninferiority criteria because the upper limit of the 95% CI (21%) exceeded the predefined noninferiority margin of 12%
- Our experts suggest starting antiplatelet agent (e.g. ASA 162-325 mg) as soon as possible after diagnosis of TIA or stroke is confirmed or if you have a high pretest probability after a plain CT has ruled out a bleed (when there is a delay to CT angiogram), understanding that there is no strong evidence for clinical benefit. Antiplatelet agents should be delayed for 24 hours in those patients receiving thrombolytics.
- Our experts recommend having a discussion with internal medicine or neurology regarding further treatment anticoagulation and/or thrombolysis given the lack of clear evidence once a the diagnosis is confirmed with CT angiogram
- Anticoagulation is contraindicated for intracranial dissections due to risk of SAH
Is there a role for thrombolysis in cervical artery dissection?
- No RCT level data showing thrombolysis has clinical benefit
- No RCT level data on endovascular therapy
- In a meta-analysis of observational studies (2016), there was no statistical difference in favourable outcomes between thrombolysis and non-thrombolysis. ICH was higher in the thrombolysis group.
Who is safe to discharge from the ED with suspected or confirmed cervical artery dissection?
For patients with stable symptoms, a normal neurological exam and only unilateral neck/head pain at present, patients can generally be safely discharged having received ASA with expeditious neurology follow up and a script of ASA until they are seen by neurology. For patients with fluctuating symptoms, new or worsening pain, or fixed neurological symptoms, they admission is indicated for further work up including an MRI and consideration for anticoagulation.
Key take home points for red flag headaches general approach and cervical artery dissections
The big five commonly missed emergency causes of headaches that cannot routinely be ruled out on plain CT/LP include: Cervical artery dissection, CVT, Idiopathic Intracranial Hypertension, CO poisoning, Giant cell arteritis
Spinal pathology may present with headache and CNS pathology may present with neck pain – include neck pathology in patient who present with headache and vice versa
Use MY BRAIN HURTS mnemonic to run through the differential diagnosis of patients who present to the ED with headache
Up to 25% of strokes in young patients are caused by cervical artery dissections – young people get strokes!
Cervical artery dissections can present with pain only without any other symptoms, and may be spontaneous or traumatic
Delayed, fluctuating and transient seemingly “non-anatomical” neurologic symptoms that range from vertigo to amaurosis fugax to large vessel stroke syndromes are not uncommon in patients with cervical artery dissection; their neurologic exam may be completely normal in the ED
Migraines cause ipsilateral neurological symptoms; carotid artery dissections cause contralateral symptoms whereas vertebral artery dissections can cause contralateral or bilateral symptoms
Examine carefully for partial partial Horner’s Syndrome which is found in some patients with carotid artery dissection
LMWH is the most commonly used antithrombotic treatment used in extracranial cervical artery dissections, but the evidence is not clear for clinical benefit compared to ASA
Patients with stable pain and normal neurologic exam can be considered for safe discharge from the ED
If in doubt after plain CT and no contraindications, if there is a delay to CT angiogram, it is reasonable give the patient ASA in the ED and a script for ASA until they see neurologist in follow-up, although there is no good evidence supporting this practice









