Podcast: Play in new window | Download
“This learning material is sourced from Emergency Medicine Cases and has been published here with permission as per creative commons copyright”
Topics in this EM Quick Hits podcast
Sarah Reid on an approach to infant vomiting (1:08)
Brit Long on orbital cellulitis essentials (10:45)
Justin Morgenstern on update on TXA for polytrauma – the PATCH trial (18:04)
Christina Shenvi on prevention and treatment of delirium (24:26)
Jason Hine on procedural skills decay (36:58)
Aaron Billin on altitude sickness (43:37)
Podcast production, editing and sound design by Anton Helman
Podcast content, written summary & blog post by Fadi Bahodi, Sarah Reid, Brit Long, Jason Hines, edited by Anton Helman
Cite this podcast as: Helman, A. Reid, S. Long, B. Morgenstern, J. Shenvi, C. Hine, J. Billin, A. EM Quick Hits 52 – Infant Vomiting, Orbital Cellulitis, Prehospital TXA in Trauma, Prevention and Treatment of Delirium, Procedural Skills Decay, Altitude Sickness. Emergency Medicine Cases. October, 2023. https://emergencymedicinecases.com/em-quick-hits-october-2023/. Accessed November 22, 2023.
Approach to infant vomiting
Infant vomiting DDx
- Structural/Surgical: pyloric stenosis, malrotation with volvulus, intussusception, incarcerated hernia, ovarian/testicular torsion, bowel stenosis/atresia, Hirschprung’s disease
- Infectious: UTI, otitis media, pharyngitis, pneumonia, CNS (see below), gastroenteritis, URTI, pertussis
- GI: GER/GERD, overfeeding, Cow’s Milk Protein Allergy (CMPA), Food Protein-Induced Enterocolitis Syndrome (FPIES)
- CNS: mass, bleed, hydrocephalus, meningitis, encephalitis, brain abscess, congenital lesion, trauma, child maltreatment
- Metabolic/Endocrine: inborn error of metabolism, adrenal insufficiency, DKA (very rare in infants)
3 key structural diagnoses in infant vomiting:
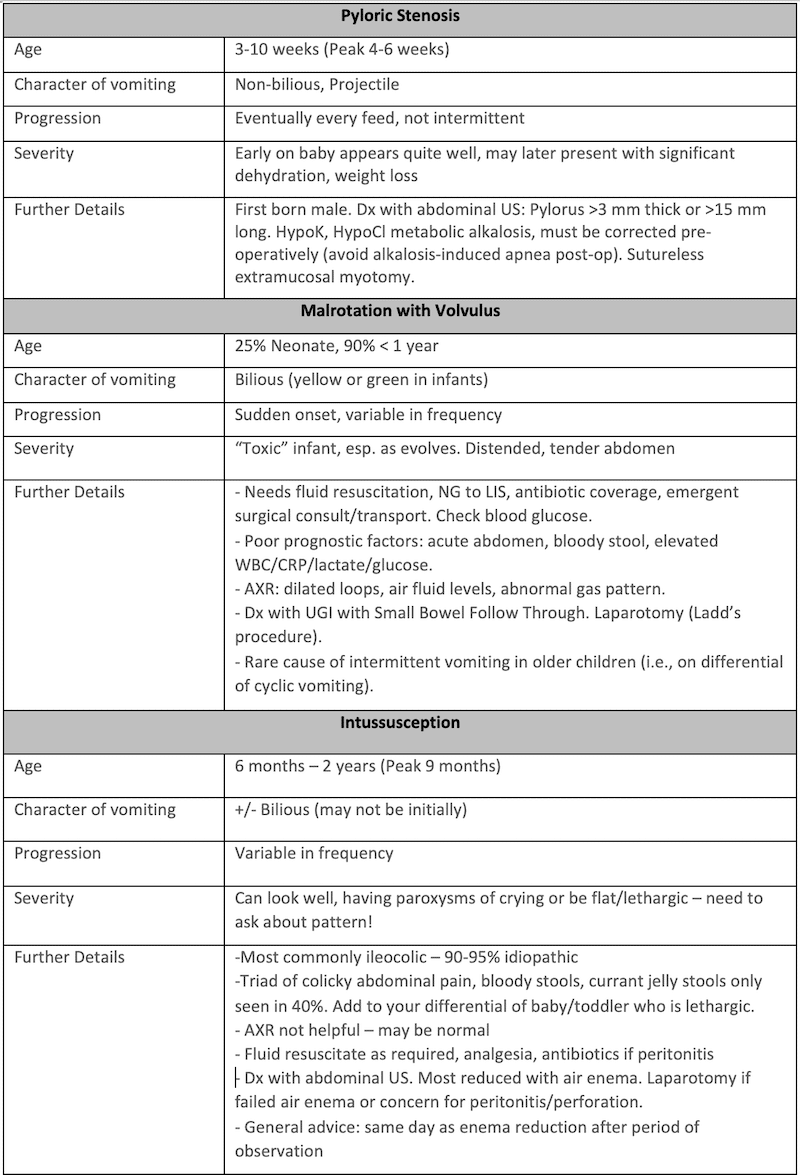
General approach to infant vomiting
- Is the baby sick or not?
- Is there fever or not? Septic workup or not?
- Characteristics and pattern of vomiting.
- Is this bilious/yellow/green/bloody?
- Is there a progression of vomiting (intermittent or every feed). Pyloric stenosis is classic for vomiting with every feed.
- Assess for behaviour sometimes linked with intussusception.
- Crying episodes, hard to console, seem in pain, drawing up their knees. Interspersed with periods of being quite well or the baby being pale lethargic. Can be (intussusception, severe illness, CNS process)
Physical exam pearls for infant vomiting
A head to toe exam is essential, including:
- Assess fontanelles for dehydration vs raised ICP
- Look in the diaper for an inguinal hernia, undescended testes, testicular torsion
The child with vomiting who is otherwise well
The normal baby with normal vitals, no blood or bile in their vomiting, vomiting intermittently, tolerating feeds in between and maintaining their hydration with an otherwise normal physical is usually an early viral illness versus GERD.
Checklist for safe discharge in infant vomiting
- Normal vitals
- No bile/blood
- Intermittent/few episodes of vomiting, tolerating feeds/oral rehydration in between.
- Well hydrated, able to maintain hydration.
- Normal full exam
Discharge instructions and disposition for infant vomiting
PCP follow-up in a few days, return to ED if persistent vomiting over a few feeds, any yellow/green/blood in vomit, less than 4 wet diapers in 24 hours, very sleepy/hard to wake, irritable/crying/pain/episodes of inconsolability, fever x 2-3 days
Orbital cellulitis essentials
The orbital septum is the differentiating factor for orbital cellulitis.
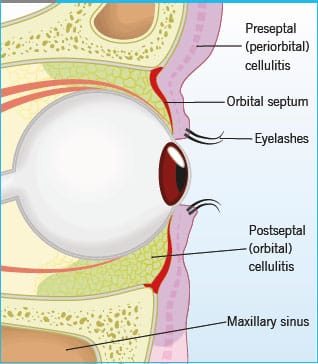
- Inflammation or infection in front of the septum is pre-septal or periorbital cellulitis. This typically involves only the eyelids.
- Orbital cellulitis is inflammation of the globe contents and surrounding soft tissues behind the orbital septum. This may lead to abscess, optic nerve ischemia, orbital compartment syndrome, and CNS infection.
- Pediatric patients are most commonly affected, and the most common underlying cause is sinusitis.
- Most cases are due to gram-positive microbes like Staphylococcus and Streptococcus.
- Red flags on history and exam: pain with eye movements, restricted or altered eye movements, photophobia, diplopia that resolves when the affected eye is closed, decreased visual acuity or color vision, RAPD, and proptosis. If one of these is present, think orbital cellulitis.
- Check intraocular pressures; there is a risk of orbital compartment syndrome with orbital cellulitis.
- Laboratory testing is not definitive. ESR, CRP, and WBC may be elevated; blood cultures are positive in less than 3%.
- The first line imaging test is CT of the brain and orbits with and without IV contrast. CT has high sensitivity and specificity, but it may be negative early in the disease. Second line imaging includes MRI of the brain and orbits with and without contrast. Ultrasound has been evaluated but is not ready for routine use.
- Management includes ophthalmology consultation and antibiotics: vancomycin plus piperacillin-tazobactam, ampicillin-sulbactam, ticarcillin-clavulanate, or a third-generation cephalosporin. If they have a penicillin allergy, use vancomycin with a fluoroquinolone.
- Some patients require operative intervention (older, diplopia, large subperiosteal abscess, intracranial involvement).
- If intraocular pressures are elevated and the patient has evidence of orbital compartment syndrome, perform emergent lateral canthotomy and cantholysis.
Update on TXA in trauma – Prehospital Tranexamic Acid for Severe Trauma: The PATCH trial
- Context: CRASH-2 was a 20,000-person trial that established clinical benefit of administering TXA in the prehospital setting for trauma patients (more detail on CRASH-2 here). Statistically significant improvement in all-cause mortality with NNT of 67 to save 1 life over 28 days. There were many more trials assessing the use of TXA in bleeding patients that showed no benefit, although for different clinical contexts (HALT-IT, CRASH-3, WOMAN, NoPAC, TICH-2)
- Methods: Double blind, placebo-controlled RCT, randomized 1307 pre-hospital trauma patients to TXA 1g IV bolus then 1g over 8hrs, or placebo.
- Primary outcome was survival with favourable neurological outcome at 6 months as assessed with the use of the Glasgow Outcome Scale–Extended (GOS-E) with a GOS-E of 5 or above being defined as favourable.
- Key results: There was no statistically significant difference in the primary outcome, however there were more survivors with poor neurologic outcome (severe disability) in the TXA group at 6months. TXA did improved all-cause mortality at 24 hours and 7 days by 4%, but with a 4% increase in vascular occlusive events.
- Commentary: The PATCH trial seams to support the findings of the CRASH-2 trial that prehospital TXA reduces early death from bleeding in severe trauma patients, but no improvement in 6 month survival with good neurologic outcome, and increased survivors with severe disability. As this trial is much smaller than CRASH-2 it continues to be reasonable to administer TXA for within 2-3hrs. Future studies should attempt to replicate CRASH-2 and find subgroups who may benefit from TXA.
First10EM deep dive on PATCH trial
Prevention and treatment of delirium in the ED
Prevention of delirium in the ED
- Identify patients with delirium and those at high-risk of developing delirium (see part 1 of this quick hits series on delirium recognition and assessment/workup of delirium)
- Avoid high-risk medications. This includes sedatives, benzodiazepines, diphenhydramine, or other medications that could potentially trigger/worsen delirium.
- Restart home medication unless contraindicated
- Treat pain, a major contributor to delirium
- Normalize hydration and body functioning; minimize NPO orders and if NPO is necessary ensure IV hydration; provide food early if no contraindication
- Mobilize the patient and minimize tethering – minimize urethral catheters, cardiac monitoring etc.
- Involve family members to reorient and support patient during their stay
- If hearing impairment/cognitive impairment, may need to repeat your plan
- Reduce ED length of stay whenever possible
- Avoid high-risk medication like diphenhydramine. It has antihistamine and anti-cholinergic properties that can worsen delirium.
- Avoid benzodiazepines when possible. Can cause sedation and paradoxical worsening of delirium. Sedation can last a very long time in older populations which can be problematic.
Treatment considerations for delirium in the ED
- Treatment of delirium involves treating underlying cause. Look for easily reversible causes that can be initiated in the ED (hypoxia, hypercarbia, hypo/hyperglycemia, hypo/hypernatremia, hypo/hyperkalemia, dehydration, severe anemia).
- Manage symptoms of delirium with non-pharmacologic interventions including verbal de-escalation, distraction (busy vests/blankets), reassurance/reorientation.
- For agitation, start with oral meds. Start low and go slow. The goal of medication is safety, not sedation.
- If on antipsychotic at home, start with that drug.
- Best antipsychotic options for agitation in older patients:
-
- Olanzapine 2.5-5.0mg
- Risperidone 0.5-1.0 mg
- Quetiapine 25-50 mg
- If the patient cannot tolerate oral medications, IM antipsychotic options include:
- Olanzapine 2.5-5mg IM
- Risperidone 10 mg IM
- If need to give IM or IV haloperidol, start with low doses 0.25 mg to 0.5 mg.
- Parkinson patients have special considerations since antipsychotics can induce extrapyramidal symptoms. Quetiapine is usually the best option; consider consulting with a pharmacist before giving antipsychotics to a Parkinson’s patient.
- Benzodiazepines should only be used as a last resort if there are no other options for safety or if treating alcohol/benzodiazepine withdrawal.
Procedural skills decay in emergency medicine
- Tactile skills decay more slowly than cognitive ones, but we do less to maintain them, especially for HALO (High Acuity, Low Occurrence) procedures. This is a set up for procedure avoidance, errors, and patient harm.
- Cognitive science teaches us that spaced repetition is important to keep ourselves competent. This training is most efficiently done with short training sessions spaced out through time. For highest performance, this is ideally done in situ (where you work). This practice can take many forms, including:
- Active video review
- Mental modeling
- Simulation- low, mid or high fidelity
- Stress inoculation is the concept of purposefully instilling small amounts of stress into the training, which has two benefits. It more closely replicates the actual clinical environment of HALO procedures and works as a powerful memory aid. Stress inoculation can be added simply by:
- Timing yourself
- Audio cues- for example alarming telemetry
- Performing in front of an audience
- Finally, remember anything is better than nothing. Anything you add today is better than your current status quo for your confidence and patient safety.
To prevent procedural skills decay, get home delivered simulation kits and video instruction via SimKit
Acute altitude illnesses
- Altitude illness life threats include:
- Acute Mountain Sickness (AMS) +/- progression to High Altitude Cerebral Edema (HACE)
- High Altitude Pulmonary Edema (HAPE)
- The partial pressure of oxygen at high altitude is greatly reduced leading to hyperbaric hypoxia
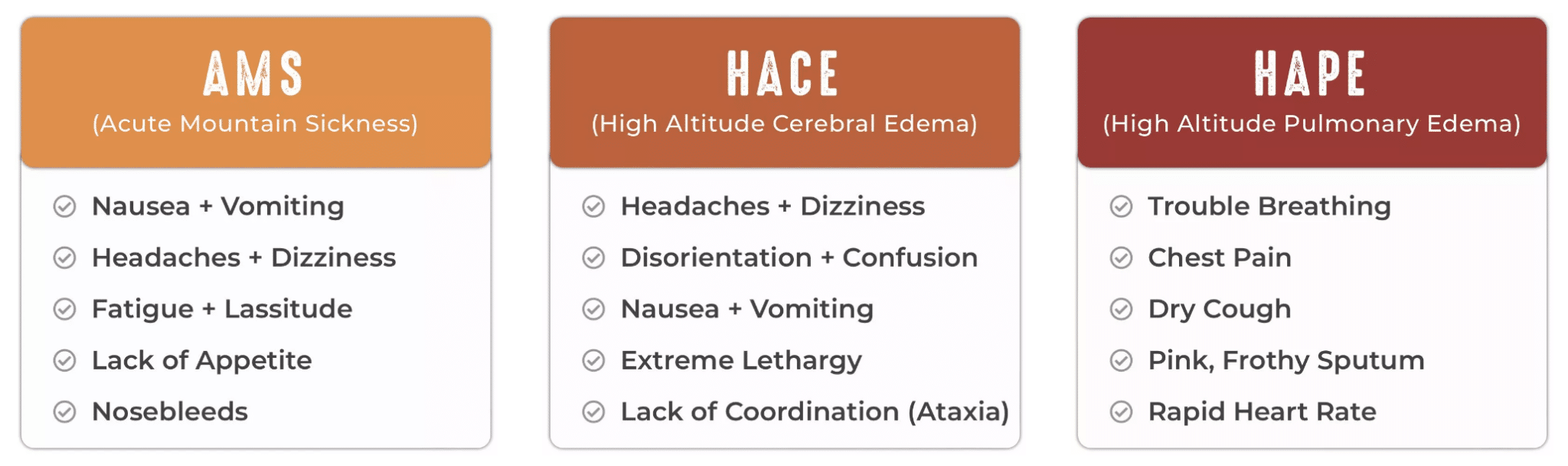
Acute Mountain Sickness (AMS)
- AMS starts with diffuse headache (which may be the only symptom and usually settles with supplemental oxygen, NSAIDs and/or acetamimophen) and can progress to cerebral edema with elevated ICP
- Avoid opioids for high altitude associated headache as opioids may depress ventilation and worsen AMS
- Diagnosis is made with a score of ≥3 points on the self-reported Lake Louis Acute Mountain Sickness Score which includes points for headache, GI symptoms, fatigue or weakness, dizziness or lightheadedness and functional limitation
- An important clinical clue to AMS is the absence of normal diuresis associated with acclimatization to high altitude
- DDx of AMS includes dehydration, hypothermia, hyponatremia, hypoglycemia as symptoms are nonspecific
- Treatment of AMS: stop ascent, descend 500-1000 meters if possible, do not resume ascent until symptoms have resolved, Acetazolimide 250mg bid x 2 days, supplemental oxygen, portable hyperbaric chamber if decent is not possible
- AMS prophylaxis: Acetazolimide 125mg bid has been shown to prevent AMS in a systematic review/meta-analysis of RCTs
High Altitude Cerebral Edema (HACE)
- Progression of untreated AMS may result in HACE
- Typically presents with ataxia +/- altered LOA + AMS symptoms at high altitude
- Other features of HACE include hallucinations, seizures, focal neurologic findings
- Treatment of HACE includes:
- immediate decent to at least 1000-3000 meters,
- dexamethasone 8mg po or IM or IV followed by 4mg q6h
- supplemental oxygen to keep oxygen saturaion >90%
- securing the airway for low/worsening GCS
- portable hyperbaric chamber if decent is not possible
- evacuation to ED ASAP
High Altitude Pulmonary Edema (HAPE)
- Early clinical clues include decreased exercise performance, increased recovery time
- Caused by hypoxic pulmonary vasocontriction and endotheleal leak
- Dyspnea on exertion progresses to dyspnea at rest, tachycardia, fatigue, weakness, lassitude, dry cough, chest pain and low grade fever; late findings include cyanosis, crackles, hemoptysis, marked hypoxemia, and altered LOA
- HAPE may co-exist with HACE
- Treatment of HAPE includes:
- immediate decent of 500-1000 meters
- supplemental oxygen or
- sustained release nifedpine 20mg q8h or 30mg q12h
- portable hypobaric chamber if decent is not possible











