פוסט זה זמין גם ב:
עברית
Written by Clay Smith
Spoon Feed
Seven variables accurately predicted community acquired pneumonia (CAP) severity in children. This now needs external validation.
Why does this matter?
Remember earlier this year, the CARPE DIEM study? We are not very good at predicting which children with CAP will develop complications, and I was lamenting we did not have a prediction tool. Lament no more! How does this new tool shape up?
Ped CAP predictor is (almost) here
This was a prospective cohort study of 1,128 children 3mo to 18y in a pediatric ED with CAP. They derived and internally validated a clinical prediction tool that performed well at predicting severity of illness.
Severity was defined as:
-
mild – discharge or hospitalization <24h with no oxygen or IV fluids
-
moderate – hospitalization <24h with oxygen or IV fluids or hospitalization >24 hours
-
severe – ICU >24 hours, septic shock, vasoactive agents, positive-pressure ventilation, chest drainage, extracorporeal membrane oxygenation, or death
The predictor variables were:
-
respiratory rate (Z-score*)
-
systolic blood pressure (Z-score*)
-
oxygenation (abnormal PF ratio**)
-
retractions (present or absent)
-
capillary refill (≥3 seconds)
-
atelectasis or pneumonia on CXR (either/or)
-
pleural effusion (present or not)
We will definitely need an MDCalc on this one. See the gnarly scorecard below. The prediction tool performed well. Sensitivity of a low score range, ≤10%–20% predicted risk of moderate to severe disease, was 91.4%–97.1%, negative likelihood ratio 0.11– 0.17.
A recent study found some children needed no outpatient antibiotics. Also, children with mild CAP had equal outcomes with 5 or 10 days of outpatient antibiotics (SAFER trial), and CAP-IT found no difference between 3 or 7 days/high or low-dose amoxicillin. This makes me wonder if we will someday use a prediction tool like this to determine not only who would benefit from hospitalization but who would benefit from antibiotics at all. Could a score ≤100, for example, mean not only discharge home but a wait-and-see antibiotic prescription?
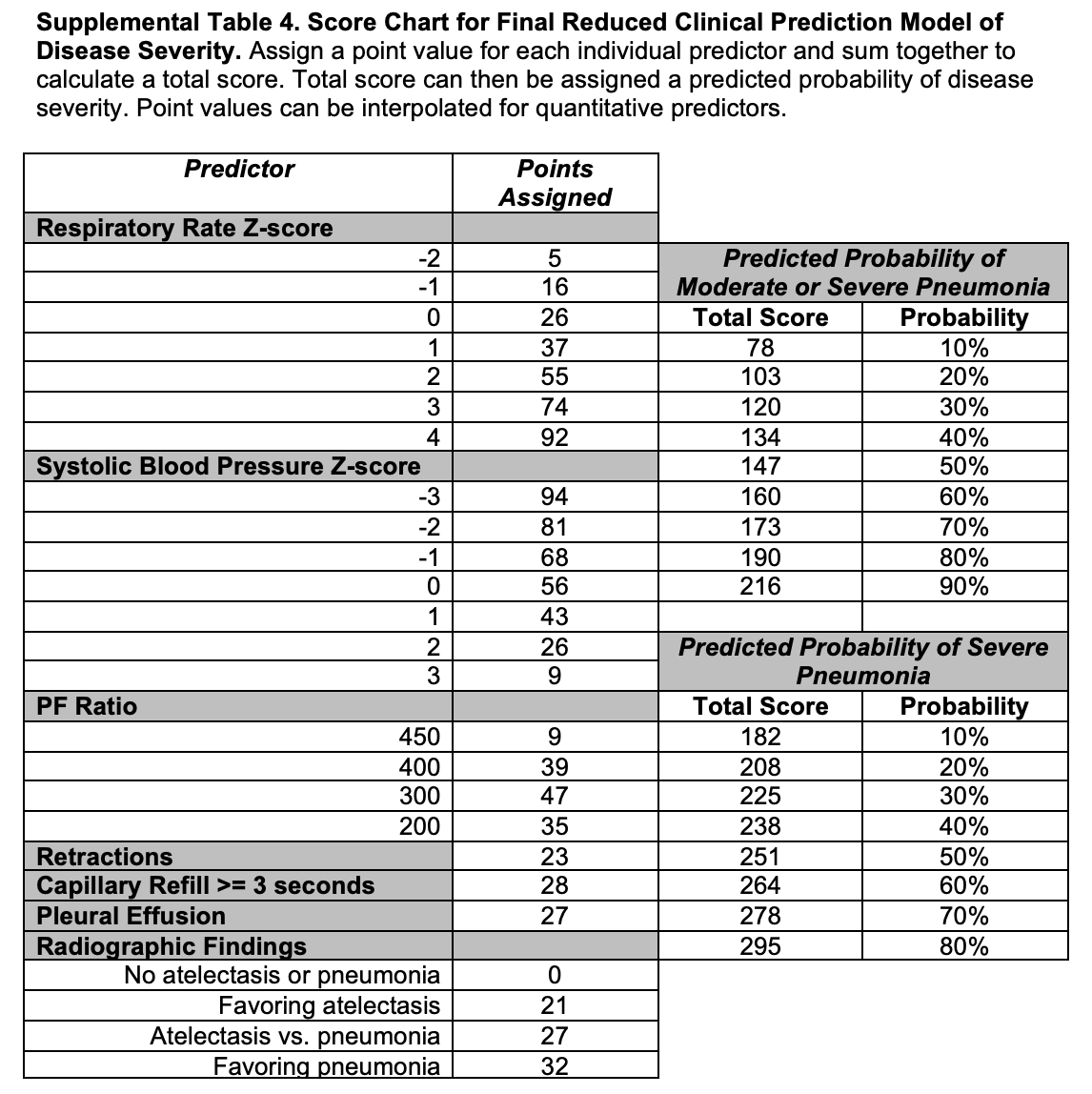
From cited article supplement
*Z-score = how many standard deviations above or below the mean.
Z-score = (x-µ)÷ meaning: (observed value – mean)/standard deviation
**PF ratio – They used SpO2/FiO2 as a proxy for PaO2/FiO2. A low number is bad. Higher is better. Example, you are now probably 99% on room air: PF = 99/.21 = 471. Imagine a patient with SpO2 90% on FiO2 70%. PF = 90/.7 = 128. Anything ≤300 is pretty bad.
Source
Development and Internal Validation of a Prediction Model to Risk Stratify Children With Suspected Community-Acquired Pneumonia. Clin Infect Dis. 2021 Nov 2;73(9):e2713-e2721. doi: 10.1093/cid/ciaa1690.





