פוסט זה זמין גם ב:
עברית
Written by Clay Smith
This is the latest on how to work up possible acute coronary syndrome in the ED.
Why does this matter?
The AHA released Chest Pain Guidelines in 2021. The ACC thought, “practical guidance was needed.”
My troponin is leaking
Here is the algorithm and my thoughts below.
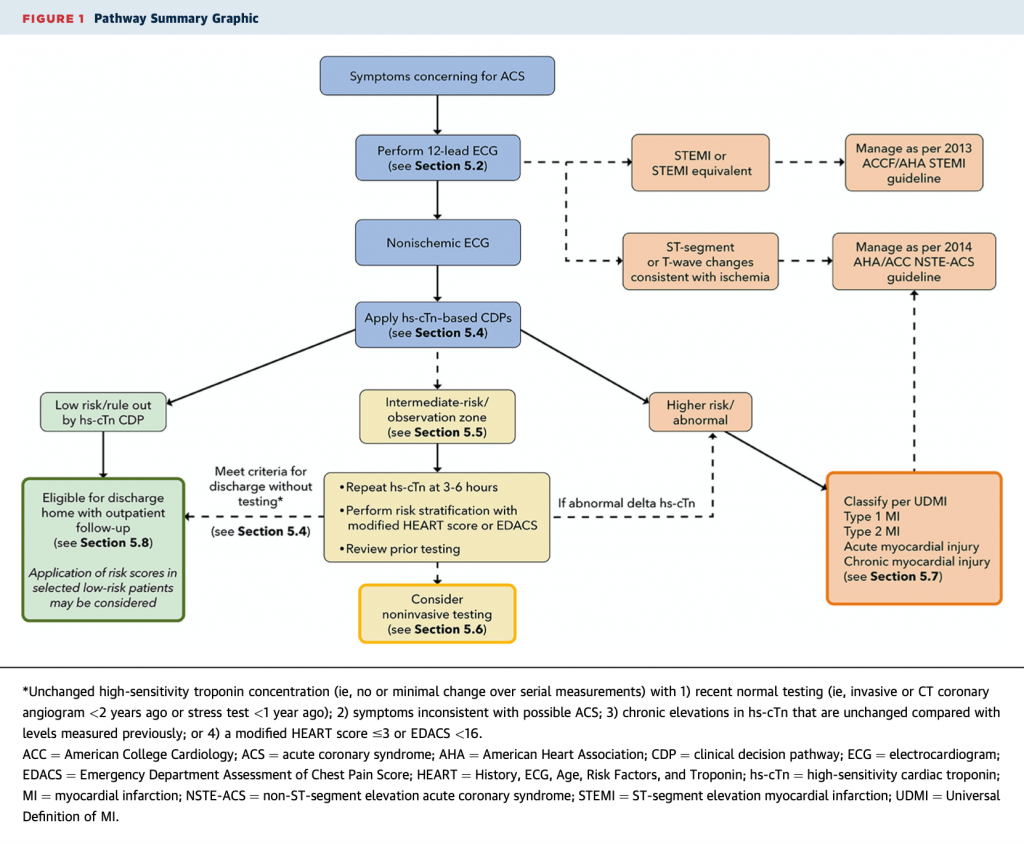
Symptoms: We say “chest pain,” but ask patients about chest discomfort (pressure, tightness, squeezing, heaviness, burning) or non-chest symptoms (pain in arm, neck, back, epigastrium, jaw). Dyspnea, nausea/vomiting, diaphoresis, fatigue, or mental status change could be ACS as well. Pleuritic, positional, or pain at a single small point on the chest wall is unlikely to be ACS. Don’t use “typical” or “atypical;” use cardiac, possible cardiac, or non-cardiac chest pain.
ECG: STEMI may be subtle in limb leads. Can you detect STEMI equivalents: posterior MI, modified Sgarbossa, DeWinter sign, and hyperacute T waves? For ischemia, would you recognize subtler aVR elevation plus global ST depression (left main disease) or Wellen’s Syndrome? Compare with an old ECG when you can.
hs-Tn-based Clinical Decision Pathways (CDP): A hs-Tn approach is recommended first, before other CDPs. Cutoff values for 99th percentile and level of quantification depend on the assay used. The European Society of Cardiology 0/1 and 0/2-hour or High-STEACS rule-outs are recommended. Assay-specific info in the full text is invaluable.
When to use HEART or EDACs: If you use conventional troponin or a patient is intermediate risk with a hs-Tn assay, use HEART or EDACS plus serial conventional troponins at 0 and 3 hours (or repeat hs-Tn at 3-6 hours). If a patient has no change in troponin/hs-Tn (i.e. a 20% increase) AND has had recent normal testing* or unchanged chronic troponin elevation or HEART is ≤3 / EDACS <16, consider discharge. If troponin rises, symptoms or ECG worsen – admit. What if patients are intermediate risk at this step? Consider non-invasive testing.
*Recent normal testing is considered an invasive or CT coronary angiogram <2 years without evidence of coronary plaque or a stress test <1 year without ischemia
Non-invasive testing: Use for intermediate risk patients. Consider coronary CTA or other testing: exercise ECG, stress CMR, stress echocardiography, or stress perfusion imaging. Use CCTA if: no known CAD, no known coronary calcification, prior inconclusive non-invasive tests, and no contrast allergy or renal dysfunction. Use other stress tests if: known CAD or calcification, contrast allergy, or renal dysfunction. CCTA may lead to more downstream testing.
So, you have a troponin leak: Is it type 1 (coronary occlusion) or type 2 (supply/demand mismatch)? Consider other causes of myocardial injury: PE, hypertensive emergency, myocarditis, stress cardiomyopathy, contusion, or recent cardiac procedure.
Source
2022 ACC Expert Consensus Decision Pathway on the Evaluation and Disposition of Acute Chest Pain in the Emergency Department: A Report of the American College of Cardiology Solution Set Oversight Committee. J Am Coll Cardiol. 2022 Oct 6;S0735-1097(22)06618-9. doi: 10.1016/j.jacc.2022.08.750. Online ahead of print.







