Written by Aaron Lacy
Spoon Feed
Decompression sickness and arterial gas embolism can present similarly and have similar treatment protocols. Decompression illness is a term that can encompass both disease processes. Recompression and hyperbaric oxygen are definitive treatments for both conditions. If you need additional help, you should contact a 24-hour expert on the topic.
Why does this matter?
Although most commonly and classically associated with recreational diving on the coasts, decompression illness can happen anywhere in the world (and off-world!). Most physicians receive limited training and education on this topic, and if missed or delayed in recognition, this treatable condition can have devastating consequences. Take some time to spoon feed yourself this topic so someday you can save a life. Just like your ascent from a deep dive, this summary is going to take a little longer than normal.
Decompressing isn’t always a good idea
Decompression illness is a modern phenomenon related to diving, aviation, medical, and aerospace technology. Let’s break down what you (the probably non-hyperbaric-trained-physician) need to know.
Definitions and pathophysiology
Decompression sickness (DCS) refers to the formation of bubbles from dissolved gas (nitrogen) that causes tissue and vascular injury as environmental pressure decreases. Arterial gas embolism (AGE) refers to when these bubbles form in the arterial system. AGE can occur in the same ways as DCS but also from pulmonary barotrauma or iatrogenic gas introduction.
Presentation and diagnosis
DCS is more common than AGE and is most common in recreational scuba diving, although the incidence (0.4 – 1 case per 10,000 dives) is low. Be most watchful of the patient who has been scuba diving and has then ascended to altitude (i.e. flying back from vacation).
There are many manifestations of DCS, with most cases having overlapping symptoms. The most commonly manifestations are musculoskeletal pain (50-65%) and patchy paresthesia (40-50%). The symptoms of DCS develop within 1-6 hours of the decompression event. AGE symptoms develop quickly and dramatically, often within 5 minutes of the decompression event and most often with cerebral involvement.
The key concept to take away here is be suspicious of DCS or AGE in any patient who has been diving, participated in any ascent to altitude (under their own power or by aviation), has gotten an intravascular procedure/had barotrauma, or is in space (probably niche, but check back in 2050).
Diagnostic Tests
To the dismay of emergency physicians everywhere (that includes me), a CT isn’t going to help you in this situation. No biomarkers or imaging studies are truly helpful or sensitive in diagnosing either DCS or AGE. Clinical presentation, history, and exam are your guide here. However, pneumothorax can co-occur with DCS and AGE during severe decompression, iatrogenic, or traumatic events, so if decompression illness is suspected, ultrasound and radiography can be helpful for ruling out pneumothorax before you place someone in a compression chamber.
Treatment
Treatment for both DCS and AGE fall into the same algorithm, so let’s focus on learning how to treat decompression illness.
First up – if you have any questions about a diagnosis, treatment, or logistical management of a patient with suspected decompression illness you should call the Divers Alert Network at +1 (919)–684–9111. Think of this as the ‘Poison Control Center’ for this type of patient.
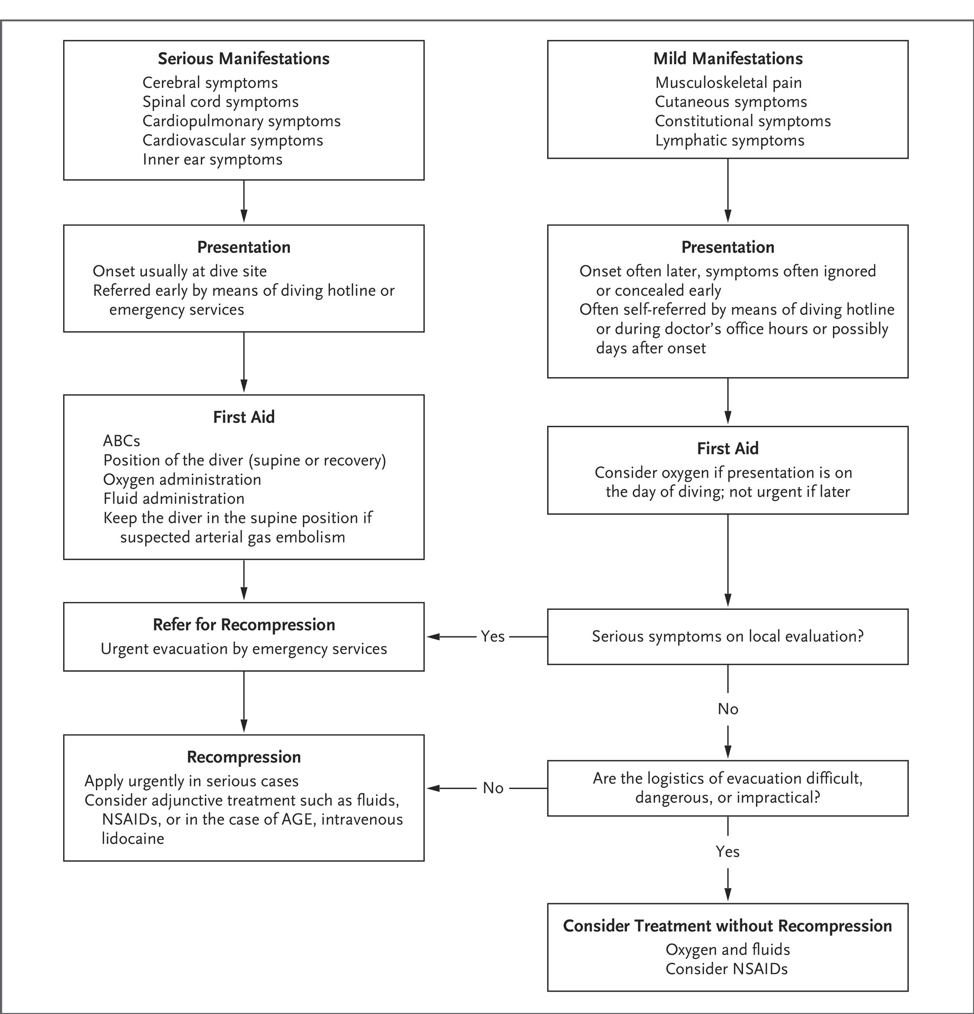
Patients should be classified into either a serious (CNS or cardiopulmonary) or mild (MSK, cutaneous, constitutional) manifestation based on symptoms. Serious manifestations are mostly likely to occur at the dive (or decompression) site or present directly from one, while mild manifestations normally are self-referring or present later.
Both manifestations require first aid. In serious cases this often involves securing the ABCs and placing the patient in the supine or recovery position. Oxygen should be administered in serious manifestations and considered in mild manifestations. There is limited utility of drug therapy and only NSAIDs have been shown to decrease the number of recompression events required for recovery or symptom plateau. Lidocaine can be used for AGE but is not standard of care. In a patient with spinal cord decompression sickness, fractionated (aka low-molecular weight) heparin should be used for VTE prophylaxis.
The definitive treatment for both serious and mild decompression illness is recompression. However, this is not always easily available or logistically simple. If a patient has a serious manifestation, you need to refer for recompression by EMS, regardless of challenges. Adjunctive treatments while arranging recompression include fluids, oxygen, and NSAIDs. If mild and logistics are difficult, dangerous, or impractical, consider treatment with fluids, oxygen, and NSAIDs alone.
Summary
“The eyes do not see what the mind does not know.” Corey Slovis
You now know who to suspect decompression illness in, how to recognize it, how to treat it, and who to call for help. Remember, this can happen to anyone; and if you never see it in a real-life patient, you will at least see it on your boards…
Another Spoonful
Here is the treatment algorithm from the cited article to download into your favorite peripheral brain.
Source
Decompression Sickness and Arterial Gas Embolism. NEJM. 2022;386:1254-1264. DOI: 10.1046/NEJMra2116554










