Clinical scenario 
A 62 year-old male involved in a high-speed motor vehicle collision was transported to the emergency department of a large community hospital. On assessment, his pulse was 110 beats/min, blood pressure 85/50 mmHg, respiratory rate 26 breaths/min, temperature 34.5 C and Glasgow Coma Scale (GCS) of 11.
The primary assessment reveals an unstable pelvis but a negative FAST examination. The ED team initiates a massive hemorrhage protocol (MHP) as part of their resuscitative efforts.
Key clinical questions
1.What is an MHP and why has the term changed from MTP?
Early administration of blood products is associated with improved outcomes in bleeding trauma patients. Every one-minute delay in the provision of blood products is associated with a 5% increase in mortality [1]. Massive transfusion protocol (MTP) is commonly defined as the transfusion of 10 or more units of RBCs in a 24 h period and is primarily focused on blood and blood component administration. In contrast, a massive hemorrhage protocol (MHP) places the emphasis on hemorrhage control, which includes [2]:
- Provision of blood components
- Maintenance of normothermia
- Use of antifibrinolytics
- Correction of coagulopathies
- Coordinated human resource response towards definitive hemostasis (ED team, core lab, blood bank, hematology, surgeons and porters)
2. What criteria should be used in the decision to activate MHP?
The decision to activate an MHP should be guided by clinical judgment, decision tools and response to treatment. Clinical scoring tools provide guidance; however, none have sufficient sensitivity and specificity for predicting the need for massive transfusion [3], Fig. 1b.
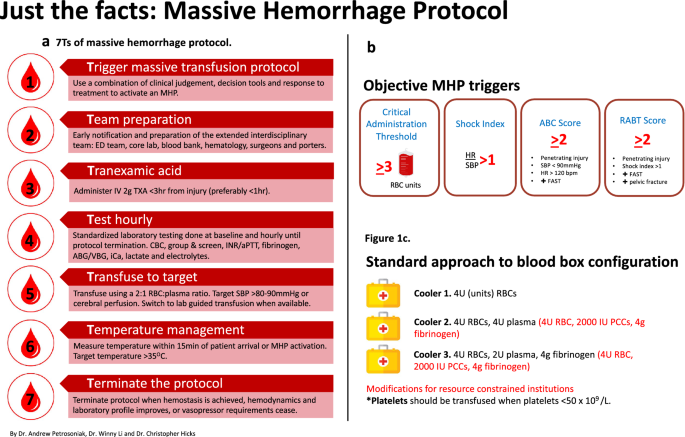
a The 7 Ts of MHP outlining key operational processes. b Objective options to guide MHP activation. c A typical composition of cooler packs in an MHP
We recommend a two-step process to MHP activation, whereby up to 3 units of RBCs are administered (critical administration threshold, CAT) [4] followed by a reassessment of the clinical response. If the CAT is surpassed or predicted to be surpassed, MHP is activated. Early MHP activation should be considered in elderly patients, those taking anticoagulation, and those with a concerning mechanism of injury predisposing to cavitary bleeding (e.g. fall from substantial height, thoraco-abdominal gunshot wounds).
3. How can an MHP be operationalized for the care of a bleeding patient?
Operational elements of an MHP can be categorized into seven critical processes known as the 7 “Ts” of MHP: Team, Trigger, Testing hourly, TXA, Temperature, Target and Termination (Fig. 1b).
The initial management of the massively bleeding patient begins with immediate RBC transfusion following a standard approach of RBC:plasma ratio of at least 2:1 [2]. Given the lack of survival benefit of a higher blood component ratio of 1:1 compared to 2:1, balancing the best evidence and resource constraints, we favor a 2:1 strategy (Fig. 1c). Consensus recommendations suggests that platelets should be transfused when platelets < 50 × 109/L or < 100 × 109/L if intracranial hemorrhage [5].
For institutions with limited plasma inventory, prothrombin complex concentrates (PCCs) 2000 IU can be substituted for coagulation factor replacement. Fibrinogen replacement of 4 g should be given with PCCs unless the fibrinogen level is known to be ≥ 1.5 g/L [5]. This strategy should be used as a bridge prior to transport to an institution capable of definitive hemorrhage control.
4. What adjuncts therapies should be part of MHP management?
Tranexamic acid (TXA)
TXA should be administered as early as possible with survival benefit decreasing by 10% for every 15 min delay in administration, and no benefit after 3 h from injury [6]. In the absence of sufficient evidence suggesting one dosing regimen is superior, administration as a single 2 g bolus IV is preferred [2].
Temperature management
An initial temperature should be measured within 15 min of patient arrival or MHP activation and be actively monitored during MHP with a goal of > 35 °C. Strategies include removal of wet clothing, increasing room temperature, infusion of all products through a blood warming device and applying external warming devices.
Calcium
Both traumatic injury and RBC transfusion can contribute to hypocalcemia, a known predictor of worse outcomes. Serum calcium should be monitored and replaced with 1–2 g of calcium chloride as indicated. A simplified approach is the administration of calcium with the first unit of RBCs and every 3 units thereafter.
Fibrinogen
Fibrinogen level should be a standard laboratory test in all MHP activations. Fibrinogen levels < 1.5 g/L are associated with increased mortality in massively bleeding trauma patients [3]. Guidelines recommend replacing fibrinogen when ≤ 1.5 g/L [5]. Fibrinogen concentrate is preferred over cryoprecipitate for its ease of administration and being pathogen-reduced.
5. What resuscitation targets should be used during MHP?
There is a lack of high-quality evidence for precise clinical resuscitation targets. Clinical markers of tissue perfusion include a combination of central pulses, capillary refill, dBP > 40 mmHg, mentation (GCS) and urine output. Practically, we strive to achieve and maintain sBP > 80–90 mmHg [7] or > 100 mmHg in the setting of significant head injury; however, targets should be considered dynamic. In parallel to resuscitation, regular coagulation tests or viscoelastic assays should be used to monitor and manage coagulopathy.
Case resolution
Our approach to managing massive hemorrhage is summarized with the 7 T framework:
Team—prior to patient arrival, the EM physician leads a team pre-brief, establishing a shared mental model and set of resuscitation priorities. MHP pre-activation is deemed not necessary, and the EM physician requests 4 units of RBCs.
Trigger—on arrival, the ABC score is < 2 while the SI > 1 and RABT = 2. Based on these conflicting findings, the team instead uses the critical administration threshold transfusing 3 units of RBCs. The patient remains unstable and MHP is activated.
TXA—2 g IV bolus of TXA is administered within 15 min of patient arrival.
Testing—blood samples are collected hourly for laboratory testing using a standardized order set.
Targets—the patient is transferred to the operating room (OR) for trauma laparotomy and pelvic fixation. The patient receives 12U RBCs, 6U plasma, 4 g of fibrinogen concentrate. The platelet level is 150 × 109/L, not requiring correction.
Temperature—the patient’s temperature is 34.5 °C on arrival prompting efforts to correct the hypothermia through the administration of warmed blood and application of a forced warm air device.
Termination—in the OR, following hemostasis and sustained hemodynamic stability, the anesthesiologist terminates the MHP and notifies all team members.
For more information on Ontario’s provincial massive hemorrhage toolkit, visit https://transfusionontario.org/en/provincial-massive-hemorrhage-toolkit/.