Written by Meghan Breed
Spoon Feed![]()
Regardless of the duration or etiology of hyponatremia, patients that have severe clinical manifestations warrant rapid administration of hypertonic saline as a 100-150 mL bolus of 3% sodium chloride or continuous infusion.
Why does this matter?
Hyponatremia (sodium level <135 mEq/L) is the most common electrolyte disorder and affects up to 35% of hospitalized patients; up to 75% develop after admission. Hyponatremia is associated with increased hospital length of stay and with morbidity, particularly in the elderly population (via cognitive defects, gait disturbances, fractures, and falls), as well as overall mortality.
For once, pass the salt…
Sodium and its anions contribute most of the particles (osmoles) dissolved in serum.
Serum osmolality = (2×Na+) + (BUN/2.8) + (glucose/18).
Unlike urea, which equilibrates across cell membranes, sodium and glucose both affect tonicity due to their low-cell-membrane permeability and, therefore, play a role in transcellular water movement. Water homeostasis is regulated by intake (thirst) and excretion (via vasopressin release – non-osmotic stimuli include pain, nausea, medications, stress). Hyponatremia develops due to excess water relative to exchangeable sodium and potassium levels (serum [Na+] = Exchangeable (Na+ + K+)/TBW) either from decreased water excretion or excessive water intake.
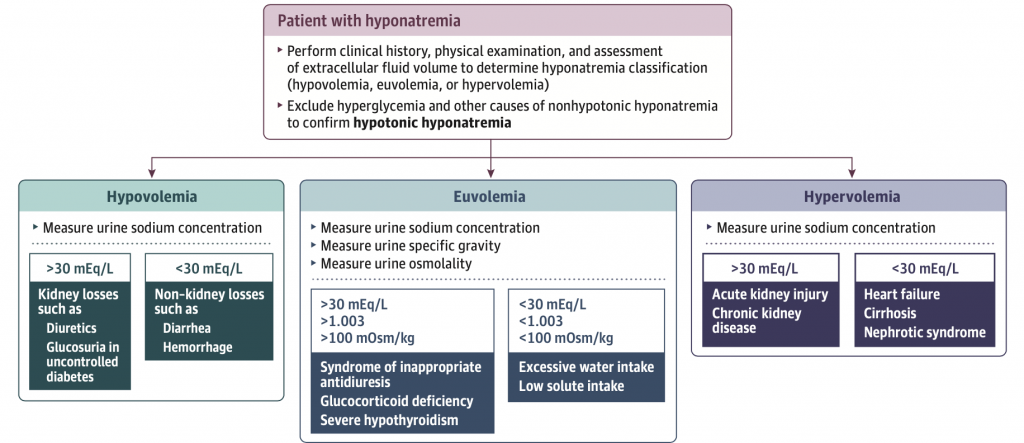
Hyponatremia is classified as mild (130-134 mEq/L), moderate (125-129 mEq/L) and severe (<125 mEq/L). Symptoms of hyponatremia depend on rapidity of onset, duration, and severity. Mild symptoms include weakness, nausea, and headache; severe to life-threatening symptoms include somnolence, seizures, and cardiorespiratory distress. After ruling out hyperglycemia and other non-hypotonic hyponatremia (i.e. exogenous solutes such as mannitol), hypotonic hyponatremia can be diagnosed and serum osmolality measured. Together, the physical exam, urine sodium, urine osmolality and urine specific gravity help differentiate between hypovolemic, euvolemic, and hypervolemic hyponatremia. See figure below.
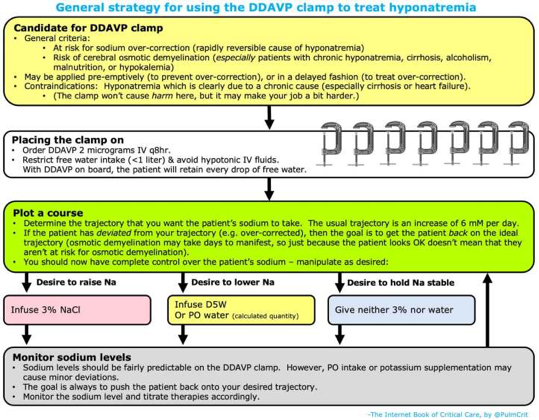
All patients with severe manifestations of hyponatremia should be treated with hypertonic saline, either a 100-150 mL bolus of 3% sodium chloride or a continuous infusion. The SALSA Trial compared these two strategies and found no difference in overcorrection; however, subsequent use of sodium lowering therapy occurred less often in the intermittent boluses group. To minimize the risk of osmotic demyelination, the desired sodium correction is 4-6 mEq/L within the first two hours, 8-10 mEq/L within the first 24 hours, and no more than 18 mEq/L within the first 48 hours. If overcorrection occurs, either desmopressin or 5% dextrose in water can be administered. Desmopressin can also be administered initially to counter the risk of overcorrection, known as the DDAVP clamp. Risk factors for development of osmotic demyelination include extreme, chronic hyponatremia, alcohol use disorder, liver disease or transplant, potassium depletion, and malnutrition.
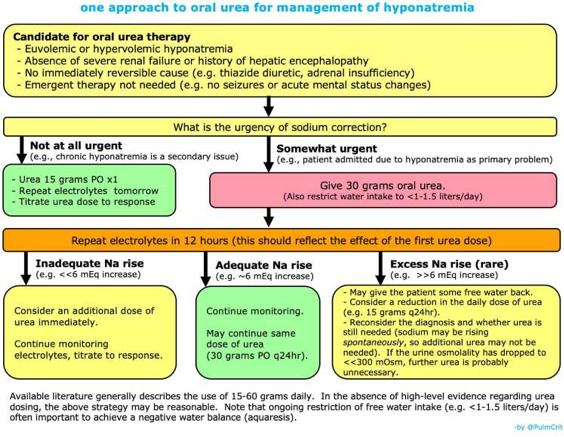
For less severe manifestations of hyponatremia, the focus should be on addressing the underlying cause. Hypovolemic hyponatremia should be treated by volume expansion with isotonic saline or balanced crystalloid, and hypervolemic hyponatremia (heart failure and cirrhosis) should be addressed by water restriction and diuretics (advanced liver disease may preclude continued use). SIADH is the most common cause of euvolemic hyponatremia and should be managed by discontinuing causative medications, water restriction, and increased solute intake (sodium chloride, protein or urea). Vaptans (vasopressin receptor antagonists) can be considered if other therapies have failed and there are no contraindications to use.
Source
Diagnosis and Management of Hyponatremia: A Review. JAMA. 2022 Jul 19;328(3):280-291. doi: 10.1001/jama.2022.11176.








