פוסט זה זמין גם ב:
עברית
Written by Jason Martinez
Spoon Feed
This article covers important pearls in the management of posterior hip dislocations along with 6 techniques all EM providers should know. Watch this hilarious YouTube video with all these techniques in under 2 minutes!
Why does this matter?
Posterior hip dislocation requires prompt diagnosis and reduction within 6 hours from time of injury to reduce the risk of complications.
It’s all in the hips…
- 90% of hip dislocations occur posteriorly. Native hips typically require a high-energy mechanism in contrast to prosthetic hips. Avascular necrosis increases significantly from 5% up to 53% 6 hours post-dislocation.
- A shortened, flexed, adducted, and internally rotated lower extremity suggests posterior dislocation, with sciatic nerve injury occurring in 20% of cases.
- Plain radiographs should be obtained initially for diagnosis and evaluation of concomitant injuries. CT plays an increasing role in these patients, as all patients with dislocations from significant trauma should receive a CT scan either before or, preferably, after prompt reduction.
- Proper procedural sedation is paramount to increase the likelihood of successful reduction, with propofol in one study being superior and with fewer side-effects compared to etomidate or an opioid-benzodiazepine combo. For poor sedation candidates, consider regional anesthesia. Initiate pain control early in these patients regardless of approach.
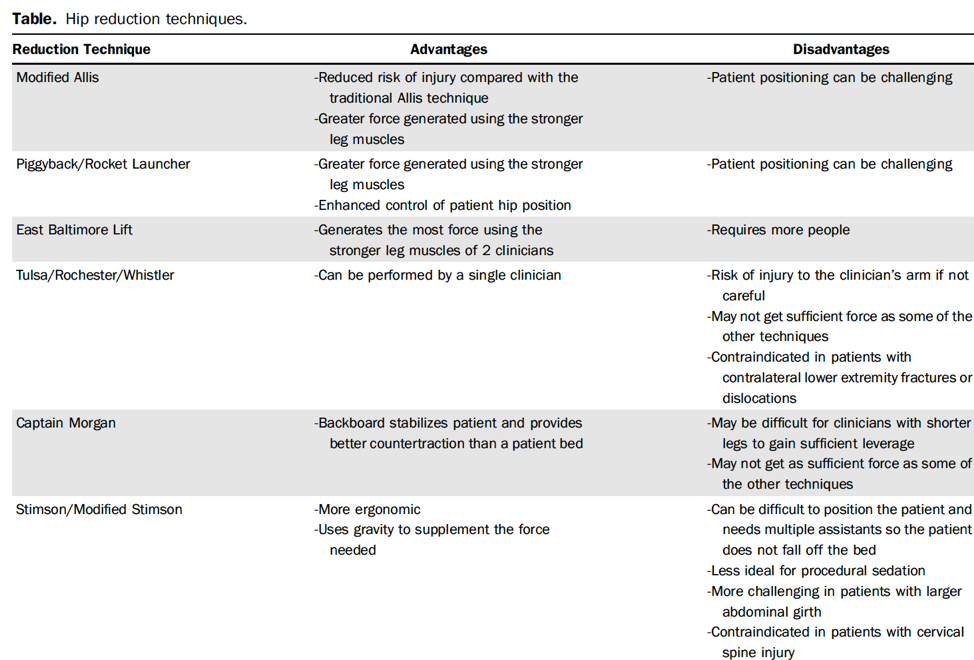
- Reduction techniques should be utilized based on provider experience; however, familiarity with all presented techniques is ideal, as certain dislocations may require varying degrees of force for reduction (native vs. prosthetic hips). Regardless of technique, follow these principles:
- Reductions need be done slowly and in a controlled fashion when applying traction.
- Forces should focus on the hip joint and avoid the knee to prevent ligamentous injuries of the knee.
- Open reductions are indicated in open dislocation, ipsilateral femoral neck fracture, or failed closed reduction.
- Post-reduction, assess the joint for stability and obtain radiographs for confirmation. Discharge is suitable with passive and active range of motion exercises with non- or toe-touch weight bearing restrictions. Consider observation for those with complications, traumatic dislocation, or inadequate access to outpatient care.
Peer reviewed by Dr. Ketan Patel
Another Spoonful
Don’t miss this hilarious YouTube video, made by UNLV residents, demonstrating all these hip reduction techniques in under 2 minutes!
Source
Managing Posterior Hip Dislocations. Ann Emerg Med. 2022 Jun;79(6):554-559. doi: 10.1016/j.annemergmed.2022.01.027. Epub 2022 Mar 9.





