***Please donate 25 seconds of your time to take our reader engagement survey! We only need about 10 more participants. Thank you to everyone who has taken it already! Here is the link: https://litannenbaum.substack.com/survey/6033390 or just click here ***
CODE BLUE OUTPATIENT RADIOLOGY CODE BLUE OUTPATIENT RADIOLOGY
“Shannon, what did the hospital voice say? Outpatient what?” you call to your charge nurse.
“Outpatient radiology, doc. I just got a priority alert from the house supervisor; the code is in ultrasound room 2. Let’s go, I’ll run with you.”
You and the code team hustle to US room 2 and see a chaotic scene. You take control of the room and assess the situation. The US tech tells you that the patient is Mrs. Chadwick. She’s a 73-year-old female who had a brain aneurysm coiled yesterday with neurosurgery. They accessed her femoral artery to get to the brain. Today, she noted bruising and pain to the groin and profound weakness. She had 2 syncopal episodes with her family while getting ready to come to the hospital. The tech tells you that she was half way through the exam when the patient suddenly passed out again and she called a code blue. She never lost a pulse, was just unresponsive but she’s starting to come to.
You and your team get a quick set of vitals (HR 55, Blood pressure 90/32, RR 18, SpO2 99% RA, Temp 99.3F) and rush Mrs. Chadwick to the emergency room for further workup and management.
When you get back to the ER, you get the patient hooked up to the monitor and see the repeat pressure is 95/40, but her mentation is getting better. She’s able to tells you a little bit more, as the team gets her situated and hands you this ECG.
“Hi Doctor, I’m just not sure what’s happening,” she tells you. “I had a very successful procedure yesterday and now I’m so weak and tired, I can’t seem to stay awake. I just want to take a nap. I have a lot of pain in my groin and it feels like my flank is hurting too. I’m not sure what’s going on. How does my ECG look?”
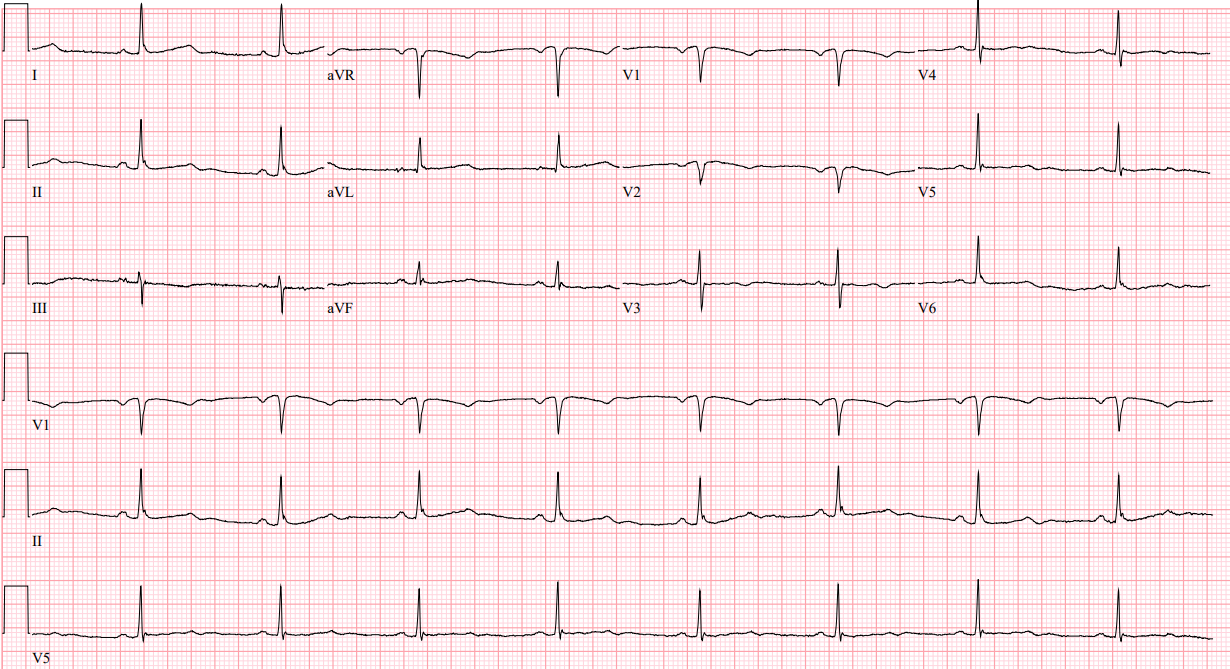
Rate: 52 beats per minute
Rhythm: Sinus bradycardia
Axis: Normal
Intervals: Looks pretty good, narrow QRS, normal PR, QTc looks ok
Morphology: Some nonspecific ST-T wave changes (T waves are pretty flat in the anterior leads) but other than that, not a ton to report
Final read: Sinus Bradycardia
“Well, ma’am, the ECG looks ok. Your heart rate is just a little slow, but nothing terrible. Let’s take a look at your access site”
When you take a look at Mrs. Chadwick’s groin site, you see a large hematoma. As you examine it more, you realize it’s pulsatile. That can’t be good. You take a look at her flank too and see extensive bruising up her side.
“Doc! Radiology is on the phone for you!” You hear Shannon call out. You excuse yourself and go take the call.
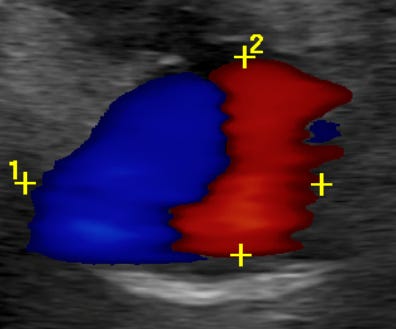
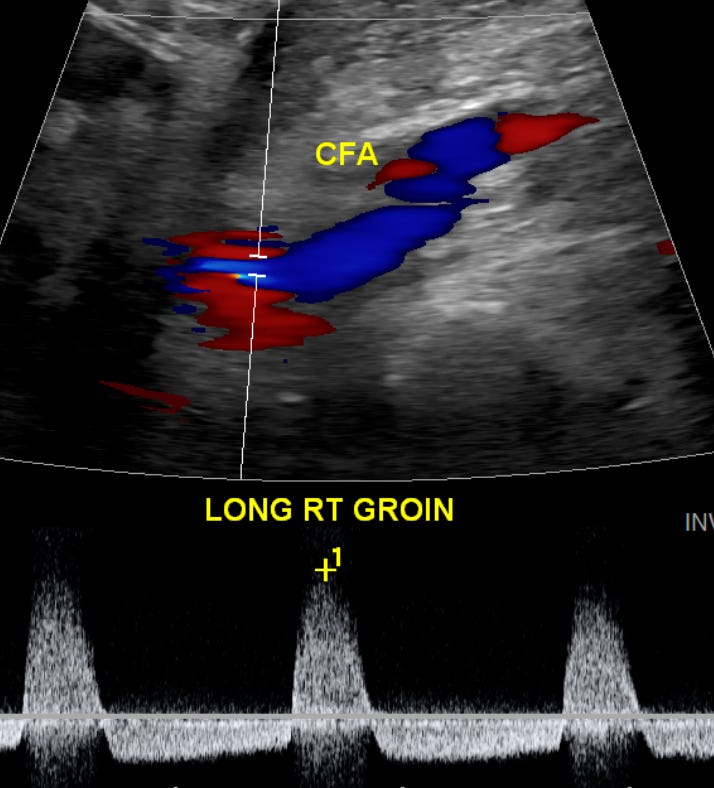
“Hey ER friend! It’s rads here. Just taking a look at the US images we got on Mrs. Chadwick before the tech called the code blue. She’s definitely got a pseudoaneurysm on that femoral artery. Here’s a quick refresher on what you’d expect to see on US for a pseudoaneurysm:”
“Pseudoaneurysms are diagnosed on ultrasound by identifying an anechoic or hypoechoic sac connected to an artery, with characteristic color and pulsed-wave Doppler showing bidirectional “to-and-fro” flow in the neck of the pseudoaneurysm.
Color Doppler demonstrates the pathognomonic “Yin-Yang” sign—a swirling pattern of blood flow within the sac. This distinctive appearance results from blood flowing into the pseudoaneurysm during systole and back out during diastole.
When using pulsed wave Doppler, the classic finding is the visualization of alternating “systolic” flow spikes above and below the baseline. Both the Yin-Yang sign on a color Doppler and the alternating spikes above and below the baseline with pulse wave Doppler are helpful in differentiating a pseudoaneurysm from a simple hematoma, which would not demonstrate internal flow.”
The tech got a great shot of the Yin-Yang sign, below:
And here is the pulse wave doppler showing alternating “systolic” flow spikes above and below the baseline:
“Alright Doc, that’s all the science I have for you, how’s she looking?”
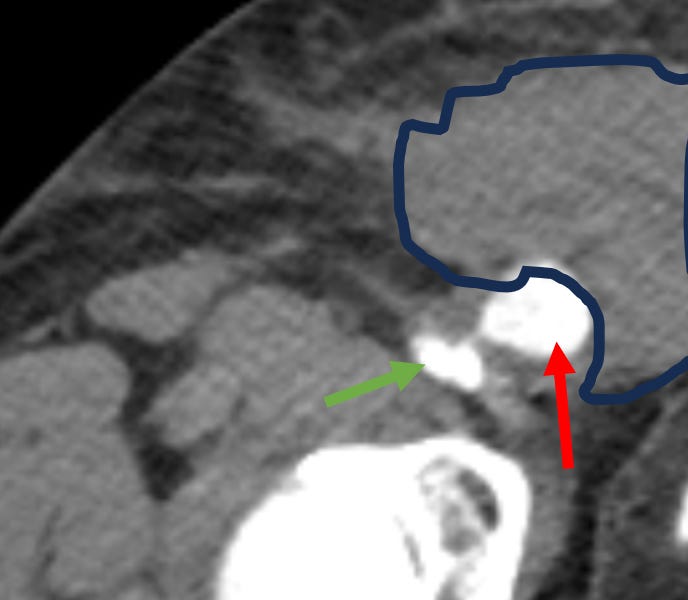
“Not good, rads, not good at all. She’s got a lot of bruising to the groin and to the flank. I wonder if the pseudoaneurysm is leaking?”
“Definitely possible. Put her in the CT scanner asap and get an angiogram, I’ll call you back when it’s done. Bye!”
You get the CTA which shows concern for an actively leaking pseudoaneurysm. The red arrow shows the aneurysm, the green arrow shows the femoral artery, and the blue freeform outline shows the hematoma around the aneurysm, which extended posteriorly, up Mrs. Chadwick’s flank.
And here is a video showing the a clip of the entire pseudoaneurysm:
Ok, perfect, we diagnosed a pseudoaneurysm, but what do we do with these patients?
Great question. **This next part is a lot of science. If you want to skip the science and just want to know what to do, jump down to the next “**” **
Well, a Cochrane Review on “Treatment for Femoral Pseudoaneurysms” was published by the Cochrane team in November of 2013 looking into optimal management of Pseudoaneurysms. The gold standard of treatment at that time was still considered surgical repair. But do all pseudoaneurysms require operative repair?
Well, no! The data isn’t the most robust we’ve ever reviewed, there were only 4 studies that were included in this review, but they looked at manually holding compression, using a device, such as the FemoStop, to hold compression, and injecting thrombin (a clotting agent) into the aneurysm to induce thrombosis.
So, what did they find? First, using an ultrasound to help guide where the compression should be focused offered no advantage to blind compression (no matter manual or device)
Now for thrombin. In the two studies that looks at thrombin (Lonn 2004 and Lui 2006), it seems to me that thrombin was more successful in causing thrombosis than compression. In the Lonn study all 15 patients who got thrombin had thrombosed within 24 hours as opposed to 2 out of 15 (13%) who thrombosed with direct US guided pressure. The patients that didn’t thrombose were retreated with pressure again, which brought the number of patients up to 6 (40%) which had thrombosed at 48 hours. Of note, all of the thrombin patients remained thrombosed when rechecked at 48 hours. Finally, those 9 left over who “failed” compression? They got thrombin and then thrombosed.
For the Lui study, 19 patients got thrombin and 19 got US guided compression. They were checked at 3 days after treatment and 7 days after treatment for pseudoaneurysm thrombosis. At 3 days, all 19 patients who had gotten thrombin had clotted, as compared with 13 (68%) who had compression. At day 7, everyone had thrombosed, no matter if you had thrombin or compression.
Interestingly, per the Cochran Review, once the data is merged, there is no statistically significant difference between treatment with compression or thrombin. Which feels a little off, after the results we just read through, right? Quoted directly from their paper, “Thrombin appears to be more effective than ultrasound-guided compression for femoral pseudoaneurysms and might be considered as the new ‘gold standard’. However, the quality of the randomization method may limit the internal validity of these results. There are potentially serious complications with thrombin, although none were reported in the included RCTs. Blind compression appears to be as effective as ultrasound-guided compression.”
If we look at where the data has gone since 2013, there was a paper published in the Journal of Ultrasonography in 2018 that looked at 135 patients with an iatrogenic arterial artery pseudoaneurysm. Of those 135, 128 (95%) pseudoaneurysms were successfully treated 24 hours after their first injection of thrombin. A second dose was given to the unsuccessful patients, resulting in a 98.5% (133/135) success rate.
**Wow! That was a lot of science. If you skipped it, start reading now to see what to do with these patients:**
But who needs thrombin (a drug injected into the aneurysm sac to cause thrombosis)? Who needs the OR? Can anyone be observed and be managed in the clinic? Well, I asked my vascular surgeon friend, and he recommended thinking of pseudoaneurysms like this:
- This needs to be in the OR now:
- Expanding hematoma
- Note: if the femoral access is higher than the inguinal ligament, the patient can develop a large retroperitoneal hematoma and have no external ecchymosis / hematoma.
- Hemodynamic instability.
- Expanding hematoma
- This could be addressed electively (Thrombin Injection):
- Pseudoaneurysm (PSA) > 2 cm
- Compression symptoms (pain)
- Large PSA causing femoral nerve palsy should be managed with open repair emergently regardless of hemodynamic status.
- Favorable features of PSA on U/S:
- Longer neck of pseudoaneurysm is associated with successful management thrombin injection
- Narrow PSA neck is a good thing (in my opinion). Neck width is viewed by some as a relative risk for thrombin injection.
- Single Lobe (or pocket) on ultrasound is associated with success.
- This could be managed conservatively: (clinic follow up, repeat duplex u/s):
- Pseudoaneurysm < 2cm
- Patients that are not on DAPT and/or anticoagulation
Case Wrap up:
After a quick discussion with vascular surgery, the team decides to take Mrs. Chadwick to the OR for an emergent repair, given her symptoms and the fact that she’s still actively bleeding into her flank.
Recap:
- In patients who underwent a recent procedure requiring arterial access, look at those access sites!
- Always think about a pseudoaneurysm after recent arterial access
- Some sites may not show a hematoma, so be careful!
- Always think about a pseudoaneurysm after recent arterial access
- On color doppler ultrasound, you can see the “Yin-Yang” sign—a swirling pattern of blood flow within the aneurysmal sac
- With pulsed wave Doppler ultrasound, the classic finding is the visualization of alternating “systolic” flow spikes above and below the baseline.
- These patients should be urgently discussed with vascular surgery, as some need emergent treatment!
- A big thank you to Drs. Jailyn Avila, Kevin Kucharski, and Jeremy Irvan for their help with this write up!
Hit me up with any questions,
Lloyd










