Written by Clay Smith
![]()
Not all pediatric bruising needs workup for a bleeding disorder. This report details not only how but when to do it.
Why does this matter?
We’ve covered high risk bruising before (TEN-4), which is bruising on the Torso, Ears, or Neck if <4 years or any bruising in infants <4-6 months. Another mnemonic is TEN 4 FACES P (i.e. injury to the Frenulum, Auricle, Cheek, Eyes, Sclera, or Patterned bruising).
Know when to test
When should we do a lab workup for a bleeding disorder in pediatric patients with bruising?
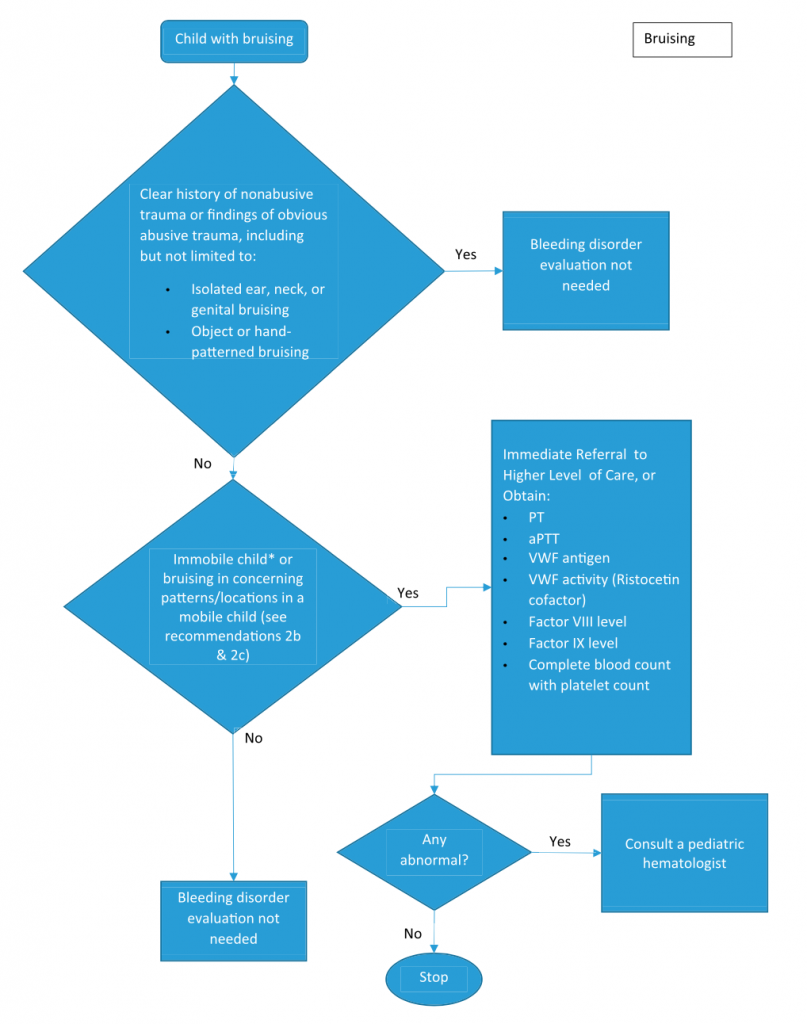
A child presents with bruising. Is there a clear non-abusive traumatic explanation, or is there obvious abusive trauma?
This does not need a lab workup.
What if there is some suspicion, not obvious abusive trauma, but may meet some TEN 4 FACES P criteria?
This is the time to either transfer the patient or do the lab workup: PT, aPTT, VWF antigen, VWF activity (Ristocetin cofactor), Factor VIII activity level, Factor IX activity level, and CBC/platelet and differential. If labs are abnormal, consult pediatric hematology.
What if a child is mobile and does not have suspicious bruising (i.e. on forehead/nose/chin (facial T), elbow, lower arms, hips, shins, and ankles)?
Lab workup is not needed.
What if a child has an ICH, specifically SDH?
Obtain CBC/platelet and differential, PT, aPTT. Congenital coagulopathies causing ICH are extremely rare: 1 in 10,000 to 1 in 1,000,000.
Other key points
Family history of bleeding disorder doesn’t preclude abuse. Suspicious-appearing, non-abusive bruising can be seen in bleeding disorders, but these disorders are very rare. Infants < 6 months with bleeding or bruising should have perinatal vitamin K administration confirmed; vitamin K deficiency will cause prolonged PT.
Source
Evaluation for Bleeding Disorders in Suspected Child Abuse. Pediatrics. 2022 Oct 1;150(4):e2022059276. doi: 10.1542/peds.2022-059276.









