Well Flec me…
***Please take 25 seconds to answer our reader satisfaction survey! Your participation will help me present ECG Teaching Cases at ACEP 2026! It’s only 6 quick multiple choice questions. Thank you to those who have already taken it!!***
“This is Medic 2915 heading your way priority one, do you copy?”
You and your charge nurse, Shannon, make eye contact and sigh. Only an hour left before the day team arrives. So close… You both hustle over to the EMS radio, “Go ahead Medic 2915, we copy,” you tell them.
“Hey Doc, we’re heading your way priority one. We have an 82-year-old male who was found confused and minimally responsive by his granddaughter this morning. He has a history of kidney failure but not on dialysis yet. He also has ‘some heart thing’ that he takes flecainide for. No history of dementia but he is extremely confused when he talks to us. Barely answering questions but when he does, he doesn’t make any sense. Blood pressure is soft, 92/40. Heart rate is a little fast at 132 and irregular. Satting 90% on 2L. Lemme send you the rhythm strip we’re seeing on our monitor. It looks really weird. Transmitting now. We’re about 5 minutes out, be ready for us! Medic 2915 out.”
You and Shannon both look at each other. “Well. Here we go. Let’s get room 8 ready…”
“Doc, here’s the rhythm strip Medic 2915 sent, it’s just printing out now,” Shannon tells you as she hands you the strip:
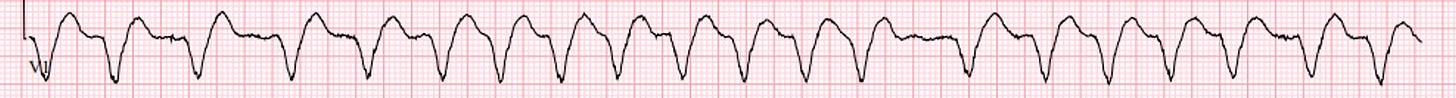
Well. That’s not good. We’re only looking at one lead but we have an irregular wide complex tachycardia. Hard to tell exactly what is going on from one lead, but I’d definitely be concerned that this patient is going to be quite sick.
“Doc, that’s the EMS door, better get ready for this patient, they are moving FAST!” You hear Shannon call to you.
“Got it, I’ll head over to room 8. Please let respiratory know we’ll probably need them. Oh! And can you give Scott and whoever else is with him on the pharmacy team a heads up that we’ll be needing their assistance too? Thanks Shannon!”
“Hey Doc! Medic 2915 here, bringing you a new friend. Not a ton more to tell you. Granddaughter told us that he’s right on the border for dialysis, but hasn’t required it yet. He’s had some GI bug for the past 2 days. She says he’s barely kept anything down, so I’m sure that’s not helping either. Moving over to your bed in 3-2-1. Good luck Doc, enjoy the end of your shift!”
You take a look at this patient and see an ill appearing 82-year-old male who is minimally responsive. The team gets IV access, gets him hooked up to the monitor, and obtains the following ECG:
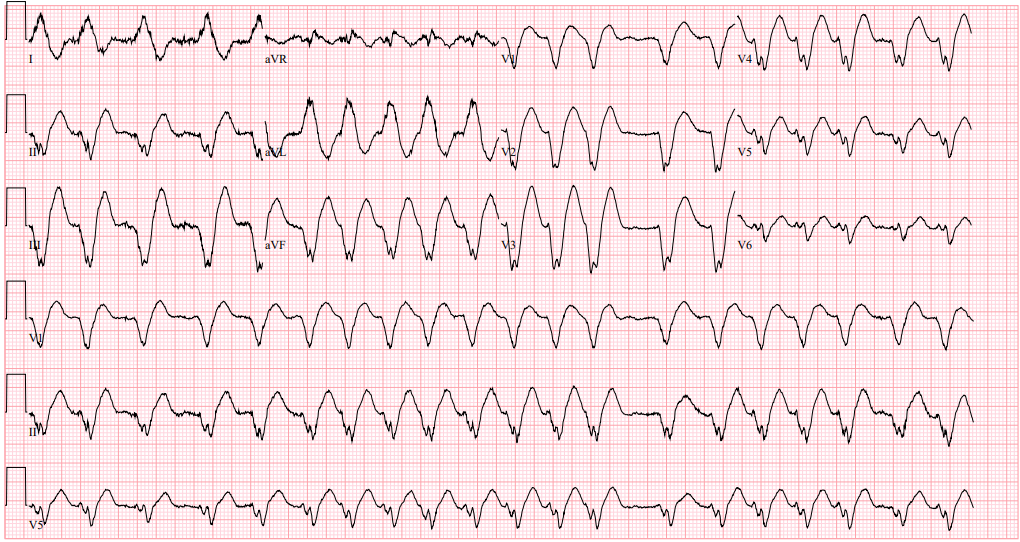
Rate: 120
Rhythm: Great question. It looks like there’s possibly some atrial activity but the rhythm is extremely irregular. It’s definitely not sinus. Either atrial fibrillation (afib) or atrial tachycardia but I’m leaning afib
Axis: Left axis
Intervals: WIDE complex QRS. I’m pretty sure I don’t see any definite PR intervals.
Morphology: Again, really wide complex QRS. It’s very irregular too. This doesn’t look good.
Final read: Irregular wide complex rhythm. I’m very concerned about this person.
“Hey Doc! We need some instructions here, what are you thinking?” You hear Shannon call out to you.
“Right, right! Ok, Let’s get him a bolus of IV fluid, run a liter in quick. Let’s also set up to intubate, he’s not really protecting his airway. With this wide, irregular rhythm, I wonder if his flecainide has reached a toxic level. It would fit, with his GI bug and baseline renal insufficiency. If he has an AKI, it can cause the flecainide to build up and cause rhythms like this. Shannon, can you put out a stat call to toxicology? I’m going to give him some bicarb, IV fluids, and get him intubated in the meantime. I also have a pretty low threshold to consider cardioversion since we don’t know what’s going on and it’s a weird looking rhythm. Thanks everyone!”
“Hey Doc! Tox is on the line, Dr. Boroughf is holding,” You hear Shannon call.
“Excellent! I just finished the intubation and we pushed that bicarb, Hey Bill! Hope you’re doing well! Can I run a patient by you? I’ve got an 82-year-old male with concern for flecainide toxicity. His ECG is in the chart but it’s a wide, irregular mess. VBG shows a pH of 7.30 and lactate 3.2. Stat Creatinine came back at 5.2, baseline is 3.2. His potassium is a little high at 5.8 too. He has a GI bug, sounds like he got an AKI and his flecainide is at a toxic level? According to family he hasn’t missed any doses. Vitals show a HR of 120-140, BP is 90/32 after a 1L bolus. Any ideas on him? Thanks!”
“Yo Doc, a call from you always means we’re about to have some fun. Flecainide, you say…? I’m pulling up the EKG now… Holy crapped out kidneys, man! I’m no cardiologist, but more points than straights is a problem. Those mile-long QRSs are definitely pointing to flecainide, that most lovely class 1c antidysrhythmic, which is blocking, like, all of the sodium channels. Wide QRS, prolonged QTc, tachydysrhythmias, hypotension, depressed mental status– the five fearsome features of flecainide.”
“Ok, great. So, what should we do now?”
“Flecainide can be super tricky, but you’re already on the right track. Sodium channel blockers deserve sodium, and sometimes lots of it. Also, since receptor binding is pH-dependent, alkalosis is your friend. Ergo, sodium bicarbonate is the first line. Because flecainide can sometimes be poorly responsive, you’re potentially going to need a lot of bicarb. So, keep your patient on the EKG machine, bring in a big box of bicarb and push it– push it real good. Your goal here is to induce a significant sodium gradient to overwhelm the blockade (so to speak), which will narrow the QRS and improve cardiac function (and blood pressure).”
“Now, the optimal amount of narrowing is uncertain. Folks often take the QRS goals of TCAs (i.e. QRS < 100 ms) and apply that generally to all sodium channel blockers, but this is a tox pseudo-axiom. All we’re looking for is some degree of improvement that coincides with an improvement in cardiac output, and if that happens at 110 or 120ms, we’ll take it. At the same time, you can consider hyperventilating the patient to induce a respiratory alkalosis, since that will kick more flecainide off the sodium channel, allowing our gradient to drive sodium more into the myocytes and improve inotropy. Also, fluids and pressors. Always fluids and pressors.”
“OK, We’re pushing the bicarb and tuning up the vent a bit. How far can we push this, and what are the next options that we should be thinking about?”
“The ceiling is what I call ‘x55’, serum sodium of 155 and pH of 7.55– anything beyond this and you’re potentially making things worse (in other ways). If you’ve hit these numbers and things are unchanged, here are the next steps:
- Lidocaine: 1-2 mg/kg bolus, followed by 1-2 mg/min infusion if responsive. The logic here is as follows: while lidocaine is technically a sodium channel blocker, it’s a class 1B, which means that it behaves differently. In this case, it rapidly cycles on the sodium channel and competes for flecainide. More on-and-off per minute means more opportunity for sodium to enter, which means a narrower QRS. Max dose here is probably about 3 mg/kg (infusion max 4 mg/min).
- Hypertonic 3% saline: If you’ve hit the pH ceiling but not the sodium cap, then you can also consider plain old 3% saline at 100 mL boluses until you hit your 155 target.”
“If that doesn’t work, then it’s time to start thinking about Intralipid or ECMO with the following considerations:
- VA-ECMO: Given that flecainide results in pump dysfunction, ECMO is a viable solution supported by a variety of case reports/series (my own experience). If the patient is a candidate (and you have the technology), it is worth considering early, before the patient arrests. (Fun fact #1, there is some literature that shows the circuit tubing may sequester free flecainide!).
- 20% Intralipid: Flecainide is highly lipophilic. There are numerous case reports detailing successful resuscitation of bad flecainide with 20% intralipid (I prefer bolus dosing of 1.5 mL/kg, repeated x 2 followed by infusion only if responsive). However, there is likely significant publication bias in this space, and it should be considered if there are no other options. (Fun fact #2: intralipid can interfere with ECMO causing fat deposition and increasing clot formation risk.)”
“Lastly, here are some things to avoid:
- Bicarbonate infusions: the amount of sodium/hour of a bicarb infusion is inadequate compared to a bolus. It will, however, result in prolonged potassium loss, which will make the QTc even longer. Instead, monitor the EKG and if the QRS is starting to widen out again, hit ‘em with a PRN bicarb push.
- Dialysis: Sadly, working kidneys or not, dialysis cannot remove flecainide.
- Amiodarone: While isolated case reports exist, amiodarone is a dirty drug that can significantly prolong QTc and is not routinely recommended.”
“Beyond that, there’s not much else to do other than hope the kidneys start doing their job. Flecainide has a long half-life, so prepare the ICU for a long night. As always, your friendly neighborhood toxicologist is just a phone call away!”
Case Wrap up:
- Flecainide is a class 1c antiarrhythmic that blocks sodium channels
- Overdoses can result in the “five fearsome features of flecainide!”
- Wide QRS
- Prolonged QTc
- Tachydysrhythmias
- Hypotension
- Depressed mental status
- Sodium bicarb and alkylosis are your first line treatments
- Use Sodium Bicarb pushes, not a drip
- Hyperventilate the patient
- Remember the ceiling of “x55”
- Sodium no higher than 155
- pH no higher than 7.55
- If bicarb pushes and hyperventilation aren’t working, consider Lidocaine, 3% Saline (if you’re still <155, but maxed out on pH), ECMO and Intralipid
- Avoid Bicarb Drips, Dialysis, and Amiodarone
- Please take our reader satisfaction survey!
- Thank you to those of you who took it already!
Thank you again Dr. Bill Boroghf for your expertise and insights! And please take a look at his substack, The Thing About Poison, with Dr. Bill Boroughf for more excellent toxicology knowledge!
Selected References from Dr. Boroughf:
Vu NM, Hill TE, Summers MR, Vranian MN, Faulx MD. Management of life-threatening flecainide overdose: a case report and review of the literature. HeartRhythm Case Reports. 2015 Dec 29;2(3):228.
Shamapant N, Edward JA, Tzou WS, Tumolo AZ. MANAGEMENT OF WIDE COMPLEX ARRHYTHMIAS DUE TO FLECAINIDE TOXICITY. Journal of the American College of Cardiology. 2023 Mar 7;81(8_Supplement):2530-.
Valentino MA, Panakos A, Ragupathi L, Williams J, Pavri BB. Flecainide toxicity: a case report and systematic review of its electrocardiographic patterns and management. Cardiovascular toxicology. 2017 Jul;17(3):260-6.
Hit me up with any questions,
Lloyd
**Looking for a dynamic guest lecture on Emergency Cardiology for your Grand Rounds? Reach out here for a lecture request by Dr. Tannenbaum. If you have reached out already, I have emailed you back. If you haven’t gotten it, please message me directly on Substack or just reply to this email.**
_________________________
Lloyd Tannenbaum, MD
APD, EM Residency
Geisinger Wyoming Valley









