Podcast: Play in new window | Download
“This learning material is sourced from Emergency Medicine Cases and has been published here with permission as per Creative Commons copyright.”
Topics in this EM Quick Hits podcast
Mike Weinstock on medmal cases: upper back pain (1:29)
Andrew Petrosoniak on traumatic pneumothorax and hemothorax decision making (27:55)
Justin Morgenstern on brain injury guidelines: risk stratification for neurosurgical consult, imaging and admission (38:23)
Andrew Tagg on management of post-circumcision bleeding (47:32)
Hans Rosenberg & Ariel Hendin on evaluation and management of CT contrast allergy (50:30)
Shawn Seregren on emotional contagion in resuscitation teams (59:30)
Podcast production, editing and sound design by Anton Helman
Podcast content, written summary & blog post by Anton Helman, January, 2026
Cite this podcast as: Helman, Petrosoniak, A. Morgenstern, J. Tagg, A. Rosenberg, H. Hendin, A. Seregren, S. EM Quick Hits 70 – MedMal Case Upper Back Pain, Traumatic Pneumothorax/Hemothorax Decision Making, Risk Stratification of ICH for Consultation, Post-Circumcision Bleeds, IV Contrast Allergy, Emotional Contagion. Emergency Medicine Cases. January, 2026. https://emergencymedicinecases.com/em-quick-hits-70-jan-2026/. Accessed January 14, 2026.
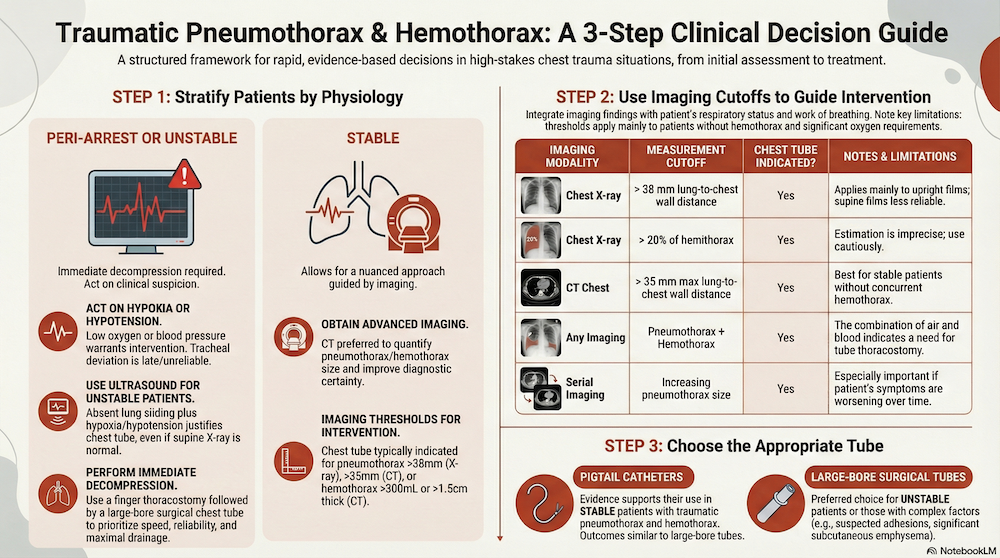
Traumatic Pneumothorax and Hemothorax Decision Making: A 3-Step Approach
This is Part 1 of a 2-part EM Quick Hits series on traumatic pneumothorax/hemothorax
Step 1: Stratify patients with traumatic pneumothorax by physiology
- Peri-arrest
- Unstable / precariously stable
- Stable
This determines urgency, imaging, and tube selection for traumatic pneumothorax.
Peri-arrest or unstable patients with suspected traumatic pneumothorax: Immediate decompression is required—often before imaging. Finger thoracostomy followed by large-bore surgical chest tube placement prioritizes speed, reliability, and maximal drainage.
- Classic signs like tracheal deviation are late and unreliable
- Hypoxia or hypotension in the presence of chest trauma is enough to act.
- For unstable or precariously stable patients, ultrasound beats auscultation; absent lung sliding plus hypoxia or hypotension is enough to act on with chest tube, even if supine CXR looks “normal” (deep sulcus sign is helpful but late and often subtle).
Stable patients allow for nuance. Imaging-based thresholds for traumatic pneumothorax help guide decisions:
-
Chest X-ray: pneumothorax >38 mm or >20% hemithorax
-
CT chest: pneumothorax >35 mm (largest lung-to-chest-wall distance)
For hemothorax, CT is preferred as size is difficult to quantify on ultrasound and chest X-ray; roughly 300 mL or pleural thickness >1.5 cm is a practical cutoff for drainage.
Stable patients generally benefit from CT imaging, which improves diagnostic certainty and decision-making.
Step 2: Imaging-Based Indications for chest tube in traumatic pneumothorax — Numeric Cutoffs
| Imaging Modality | Measurement Cutoff | Chest Tube Indicated? | Notes & Limitations |
|---|---|---|---|
| Chest X-ray | > 38 mm lung-to-chest wall distance | Yes | Applies mainly to upright films; supine films underestimate |
| Chest X-ray | > 20% of hemithorax | Yes | Estimation is imprecise; use cautiously |
| CT chest | > 35 mm maximal lung-to-chest wall distance (axial view) | Yes | Best applied in stable patients without hemothorax |
| Serial imaging | Increasing pneumothorax size | Yes | Especially if symptoms evolve |
| Any imaging | Pneumothorax + hemothorax | Yes | Blood + air → tube thoracostomy |
*These thresholds apply primarily to patients without hemothorax and without significant oxygen requirements.
*Decisions should integrate imaging findings with respiratory status and work of breathing.
Step 3: Tube choice for traumatic pneumothorax and hemothorax
Evidence supports pigtail catheters for stable patients with traumatic pneumothorax and hemothorax, with similar outcomes to large-bore tubes. However, large-bore surgical tubes remain preferred in unstable patients, those with suspected pleural adhesions, significant subcutaneous emphysema, or complex injury patterns.
Risk Stratification of Traumatic Intracranial Hemorrhage for Consultation, Admission & Repeat Imaging
The AAST Brain Injury Guidelines (BIG 1–3) stratify traumatic intracranial hemorrhage by clinical risk and bleed characteristics to reduce unnecessary neurosurgery consults, repeat CTs and admissions while maintaining patient safety. Risk assignment is based on neurologic exam, intoxication status, anticoagulation, and bleed characteristics.
- Any neuro abnormality → high risk.
- Intoxication bumps risk (often at least moderate).
- Anticoagulants/antiplatelets tend to push patients into higher-risk pathways in many versions—be cautious and localize to your system.
- Prospective data show zero neurosurgical interventions in BIG 1 (low risk) and BIG 2 (moderate risk) patients, but some low- and moderate-risk patients demonstrate radiographic progression without clinical deterioration.
BIG 1 (low risk): small, simple bleeds, perfect neuro exam, no intoxication, no anticoagulants → in the study there were no neurosurgical interventions and very low rates of progression, but the data are still limited and confidence intervals wide.
BIG 2 (moderate risk): normal exam but larger bleeds or higher‑risk features → admit, repeat exam and CT; neurosurgical consultation is not mandatory up front, as neurosurgery interventions were 0% in this group despite ~7% radiographic progression.
BIG 3 (high risk): any neuro abnormality, anticoagulation/antiplatelet use (including aspirin), or larger/more complex bleeds → neurosurgery consult, admission and repeat CT; this group had high rates of clinical deterioration, progression and neurosurgical intervention.
Pragmatic approach:
-
BIG 1 (low risk): consider observation + reassessment; discharge only if your local system supports it and follow-up is reliable.
-
BIG 2 (moderate risk): admission often reasonable; consider repeat imaging selectively (progression isn’t zero).
-
BIG 3 (high risk): neurosurgical consult + admission + repeat imaging.
Practical indications to call neurosurgery + admit + repeat CT (BIG-informed)
| Decision | Practical triggers | |
|---|---|---|
| Call neurosurgery now | Any abnormal neuro exam, clinical deterioration, or CT/high-risk features consistent with BIG-3 |
|
| Admit for observation | BIG-2 or BIG-3 (e.g., intoxication, concerning comorbidity, bleed pattern/size above “minor”) |
|
| Repeat CT | BIG-3 routinely; consider in selected BIG-2 (especially if you’re admitting anyway and progression risk is a concern) | |
| ED obs then discharge | BIG-1 (strict low-risk criteria) after ~6h observation if neuro exam remains normal and no clinical worsening |
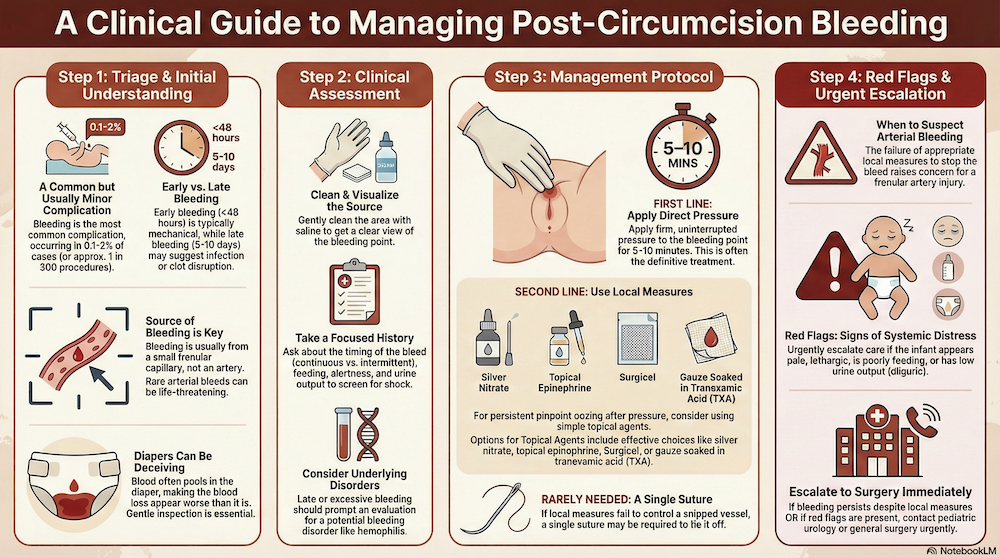
Management of Post-Circumcision Bleeding in Infants: Simple Measures & When to Escalate Care
Assessment of post-circumcision bleeding
- Early post‑circumcision bleeding is the most common complication (≈0.1–2%), usually occurs within 24-48hrs from a small frenular capillary rather than an arterial source, and is visually dramatic but often minor. Arterial bleeds, however, are rare and can be life-threatening. Early bleeding (<48 hours) is usually mechanical; late bleeding (5–10 days) suggests infection or clot disruption.
- Late or excessive bleeding should prompt evaluation for bleeding disorders.
- Focused history should clarify timing (continuous vs stopped and restarted), feeding, urine output and overall alertness to screen for clinically significant blood loss or evolving shock.
- Blood often pools in the diaper and looks worse than it is—gentle inspection is essential.
- Clean the area with saline to visualize the source.
Management of post-circumcision bleeding
- Direct pressure for 5–10 uninterrupted minutes is first-line and often definitive.
- Persistent pinpoint ooze after proper pressure can be managed with simple local measures. Options include silver nitrate and/or topical epinephrine, Surgicel or TXA‑soaked gauze.
- Failure of local measures raises concern for frenular artery bleeding. Escalate urgently to surgery (peds urology or general surgery, depending on local setup) when bleeding does not stop despite appropriate local measures, or in any child who appears pale, lethargic, poorly feeding or oliguric.
IV Contrast Allergy: Retiring Steroids, Embracing Evidence
Modern iodinated and gadolinium contrast agents are remarkably safe. Contrast agents used after 2000 are significantly safer than older formulations.
True contrast hypersensitivity is rare, most “contrast allergies” are misclassified, and routine steroid premedication should be abandoned.
How common are true allergic reactions?
- Immediate hypersensitivity reactions (HRs) to modern iodinated contrast: ~0.2–0.7%
- Severe reactions (anaphylaxis): ~0.02%
- Delayed reactions (mostly rash): ~0.05%
- Gadolinium reactions are even rarer; true anaphylaxis is extremely uncommon
Shellfish or iodine allergies are not contrast allergies.
Many “contrast allergies” represent physiologic or non-allergic reactions.
Longstanding steroid premedication protocols persist despite weak, outdated evidence derived from older high-osmolar contrast agents. Contemporary data show:
- Steroids do not reliably prevent severe reactions
- The number needed to treat to prevent one severe reaction is extremely high
- Premedication causes delays, longer hospital stays, and real harms (infection, VTE, fractures)
Contrast switching
- The single most effective strategy to reduce repeat reactions is contrast switching to a chemically different agent, reducing recurrence risk by ~60%.
- More effective than steroids or antihistamines
- Works for both iodinated contrast and gadolinium
Which antihistamines are best for treatment of true mild IV contrast allergy?
- Second-generation antihistamines (e.g., cetirizine, loratadine)
- Helpful for mild prior reactions
- Low risk, rapid onset
- First-generation antihistamines (diphenhydramine) are not recommended due to sedation and side effects
Poor documentation is the biggest barrier to safe imaging—always record the exact contrast agent, reaction type (immediate vs delayed), severity, treatment required, and outcome.
Bottom line: switch contrast agents, document accurately, and stop reflex steroid premedication.
Emotional Contagion in Team Resuscitation
Resuscitations are not emotionally neutral environments. Emotional contagion describes how tone, pace, and affect spread unconsciously through teams, shaping the emotional climate of the room. The emotional tone of a resuscitation is strongly influenced by the team leader. Leaders often underestimate how their tone affects team performance. A rushed or sharp tone amplifies anxiety, cognitive overload, and error. Calm, firm leadership steadies performance—even when decisions are complex or stakes are high. Simple, trainable behaviors help regulate the room:
- Pause before speaking
- Take a single breath before giving the next order
- Lowering your voice — not raising it — improves clarity and control.
- Structured summaries reset both cognition and emotional tone.
- Anchor yourself by making eye contact with the calmest person present
Importantly, leadership is shared. Nurses, recorders, and respiratory therapists can actively dampen rising tension with neutral phrasing and steady updates. Leadership skills require deliberate practice, often recognized after simulation.
Bottom line: emotional regulation is not “soft skills”—it is a patient safety intervention.