Podcast: Play in new window | Download
“This learning material is sourced from Emergency Medicine Cases and has been published here with permission as per creative commons copyright”
Nondisabling stroke is where Emergency Medicine earns its keep. The threats are quieter, the windows are wider, and the misses—especially in younger and female patients—are more common. In this Part 2 or our 2-part podcast update on ED stroke management with Dr. Katie Lin and Dr. Walter Himmel we explore non-disabling strokes, where symptoms are mild enough that patients can continue daily activities if deficits persist. Yet, non-disabling does not mean benign. Nondisabling strokes occupy the same ischemic continuum as high risk TIAs and carry a substantial risk of early recurrent disabling stroke. In this EM Cases podcast we answer questions such as: Which patients with non-disabling stroke can safely be discharged from the ED with prompt follow-up and which require urgent investigation or admission? Which stroke mimics do we need to be on the look out for and how do we identify them at the bedside? How dangerous is thrombolysis in a patient with presumed stroke who turns out to be a stroke mimic? What are the key distinguishing features between a stroke and functional neurologic disorder? What are the most common causes of stroke in young people that we commonly miss? How does stroke etiology dictate the management pathway? What are the indications for carotid endarterectomy in patients with nondisabling stroke and what is the ideal timing of the endarterectomy? When is dual antiplatelet therapy vs single antiplatelet therapy vs anticoagulant therapy indicated? What is the best medication strategy for the patient on a DOAC for atrial fibrillation who presents to the ED with a nondisabling stroke? For patients not on a DOAC for atrial fibrillation who come in with a stroke, when is it safe to start anticoagulation? and many more…
Podcast production, sound design & editing by Anton Helman; Voice editing by Braedon Paul
Written Summary and blog post by Anton Helman, edited by Katie Lin, November, 2025
Cite this podcast as: Helman, A. Himmel, W. Lin, K. Nondisabling Strokes Recognition and Management. Emergency Medicine Cases. November, 2025. https://emergencymedicinecases.com/nondisabling-strokes-recognition-management. Accessed November 15, 2025
Disabling vs nondisabling strokes
Nondisabling stroke accounts for a substantial proportion of ED cerebrovascular presentations. Although clinical deficits are mild, the 30-day risk of neurologic deterioration or disabling stroke is about 4-5%. ED priorities include precise phenotyping, urgent vascular imaging when indicated, early secondary prevention, and reliable short-interval follow-up. The key operational pivot is from “major/minor” toward disabling vs nondisabling—a distinction that determines whether to activate reperfusion pathways or pursue prevention-first pathways. Nondisabling stroke is where quiet presentations carry big stakes. Deficits may be subtle, windows feel wider, and the risk of being lulled into false reassurance is real—especially in younger patients and women.
Pitfall: a common pitfall is getting lulled into a false sense of reassurance for expedited workup when a patient presents with a nondisabling stroke. While nondisabling strokes do not require as rapid workup and treatment as disabling strokes, urgent workup and management should still be a priority.
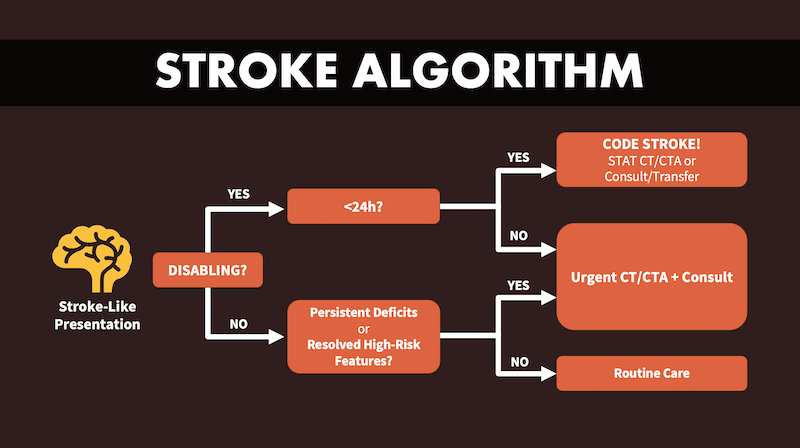
As discussed in Part 1, The very first decision is whether the symptoms are disabling vs nondisabling, not whether the presentation is consistent with a “major vs minor” stroke. Disabling means the deficit(s)—if persisted—would compromise independence: language that prevents functional communication, dominant-hand motor weakness that prevents ADLs or work, gait failure, major visual field loss, or depressed consciousness. Nondisabling implies that, even if the deficit remained, independent living would still be possible (e.g., mild facial droop, subtle sensory change, small visual field cut that doesn’t affect reading/driving, mild dysarthria without aphasia). The classification determines tempo: disabling strokes get immediate CT and stroke-protocol CTA to consider reperfusion; nondisabling strokes still demand urgent prevention—non-contrast CT now to screen for intracranial hemorrahge, CTA soon thereafter—but the pathway is focused on stopping the next event.
Source: Dr. Katie Lin’s SYNAPSE: EM Neuro Essentials Course (www.SynapseCourse.com)
Stroke miss rate and mimics – the 10% rule
Emergency physicians miss approximately 1 in 10 strokes. Short term morbidity and mortality are 8 fold higher in missed strokes. Conversely, a similar proportion of “strokes” turn out to be mimics. Recognizing the difference is critical for avoiding both under- and overtreatment.
Common stroke mimics
- Peripheral vestibular disease (vertigo)
- Metabolic or toxic states (hypo/hyperglycemia, hyponatremia)
- Seizures and post-ictal paresis (Todd’s paralysis)
- Atypical migraine
- Functional neurological disorder (FND)
Distinguishing features of stroke vs stroke mimics
| Mimic vs Stroke | Key Clues |
|---|---|
| Onset | Stroke: abrupt and maximal at onset; Mimic: gradual, spreading (“marching”) symptoms |
| Symptom type | Stroke: negative symptoms (loss of function); Mimic: positive symptoms (tingling, flashes, jerks) |
| Distribution | Stroke: neuroanatomically adjacent (face-arm or arm-leg); Mimic: patchy or shifting |
| Laterality | Stroke: unilateral; Mimic: often bilateral or inconsistent |
| Associated signs | Stroke: objective focal deficits, asymmetric reflexes, pronator drift; Mimic: variable effort, inconsistency, distractibility |
- Check capillary glucose early—hypoglycemia can mimic stroke.
- Always walk test and check truncal ataxia; missed posterior strokes often result from incomplete cranial nerve and gait testing.
Functional Neurologic Disorder (FND) – How to distinguish from stroke
Functional presentations can mimic stroke. The key is inconsistency and distractibility.
Bedside Clues for Functional Neurologic Disorder
- Pronator Drift Test: True central weakness causes pronation + drift; functional weakness often drifts without pronation.
- Give-way weakness: Inconsistent effort, especially when resistance is removed at random intervals by the assessor
- Hoover’s Sign: Lack of contralateral leg extension effort when testing hip flexion.
- Variable sensory distribution: Inconsistent changes over minutes or shifts sides.
- Distractibility: Symptoms disappear when attention is diverted.
Pitfall: Functional ≠ feigned. Up to 60% of patients with functional presentations have underlying organic disease—always rule out stroke first. Avoid diagnosing a “functional condition” in a patient without prior objective testing and/or neurologic consultation. Err on the side of stroke until proven otherwise. FND features do not exclude stroke.
Stroke mimic thrombolysis – is it dangerous?
Data show very low rates of hemorrhage (0–1%) when thrombolytics are given to stroke mimics as compared to the 3–5% seen in true strokes.
Thus, for disabling presentations, it’s safer to err on the side of treating as a potential true stroke when in doubt, including shared decision-making, informed consent when possible, and timely specialist consultation.
Why we miss strokes in young people
Strokes in the young are rare but can be devastating when missed. Approximately 13–18% of all strokes in North America occur in individuals under the age of 50. This proportion has increased over the past two decades. Younger patients are more likely to be labeled migraine, anxiety, or “functional”—particularly women—despite a vascular event. Etiologies also differ: dissection, PFO-related emboli, hypercoagulable states, and intracranial disease figure more prominently, yet we often default to “too young for stroke.”
- Cognitive traps: “too young,” prior migraine history, normal early CT, “clean” initial CTA.
- Correctives: keep stroke on the list for patients in their 20s–40s with sudden negative symptoms; do the walk test; order CTA head/neck when the story fits; avoid over-reassurance from normal early imaging if symptoms persist.
- Etiology awareness: dissection and cardioembolism are a more prominent cause of stroke in younger patients; escalate vascular and cardiac evaluation accordingly.
Etiologies of stroke in young adults
- Cervical artery dissection (carotid or vertebral)
- Patent foramen ovale (PFO)
- Sickle cell disease
- Hypercoagulable states and genetic disorders
- Atherosclerosis, increasingly seen in 20–40-year-olds
- Rare causes – including anaphylaxis-induced stroke (histamine-mediated vasospasm similar to Kounis syndrome).
Bottom line: Any sudden focal neurological deficit in a young person should be treated as a stroke until proven otherwise.
TIA and nondisabling stroke – same urgency, same treatment
Non-disabling strokes and TIAs share pathophysiology, prognosis and treatments. The DOUBT study found that 13% of TIA presentations as short as 5 minutes in duration are subsequently found to have evidence of stroke lesions on MRI. 2-17% of patients with TIA or minor stroke suffer a subsequent disabling stroke within 90 days, most within 48 hours.
High-risk TIA features: the death of the ABDC2 score
The ABCD2 score lacks sufficient sensitivity and specificity to reliably stratify short-term stroke risk after TIA, particularly for identifying patients at very low or very high risk. The score does not account for critical high-risk features such as ipsilateral large artery stenosis, atrial fibrillation, recurrent or crescendo TIAs, or imaging evidence of acute infarction, all of which substantially increase early stroke risk independent of ABCD2 score. As a result, patients with low ABCD2 scores may still harbor significant vascular pathology and face substantial risk, undermining the score’s utility for disposition or management decisions. Instead, current best practice focuses on clinical features to risk stratify patients. These are the features that predict a subsequent disabling stroke and mandate urgent imaging and treatment:
- Speech disturbance (aphasia, dysarthria)
- Motor weakness
- Vision loss
Why persistent deficits in nondisabling stroke and high-risk features in TIA matter
Persistent nondisabling deficits and resolved high-risk features share the same message: active cerebrovascular pathology with high risk for early subsequent stroke. A persistent deficit—even when “mild”—raises the pretest probability of a treatable lesion such as symptomatic carotid stenosis, intracranial atherosclerosis, or cervical artery dissection, and the opportunity for secondary prevention. Resolved high-risk features—true motor weakness (often described as heaviness), speech or language disturbance, major visual field loss, or depressed consciousness—suggest potentially high risk vascular territory at risk for susequent stroke from ongoing vascular pathology. Either scenario should trigger urgent head CT to exclude hemorrhage, early CTA head and neck to define the vasculature, and immediate antithrombotic decisions. The goal is to prevent the next stroke event, which is at highest risk within the first 48 hours to one week.
Stroke etiology and treatment pathways (Rule of 4s)
-
~¼ Large-artery atherosclerosis (carotid/intracranial):
- Clues: prior TIA, bruits, focal cortical signs.
- Action: CTA head/neck to find carotid stenosis/dissection.
- CEA: symptomatic ICA 70–99% stenosis likely to need surgery/stenting; 50–70% often considered for surgery/stenting.
- Timing: avoid the first 48 h after stroke; target within ~2 weeks before benefit wanes.
- Antithrombotic while waiting for CEA (pre-op): single antiplatelet plus statin and risk-factor control.
-
~¼ Lacunar/small-vessel:
- Clues: pure motor/sensory syndromes, small deep infarcts.
- Action: DAPT and aggressive risk-factor management.
- ~¼ Cardioembolic (AF, cardiomyopathy, valve/aortic thrombus, PFO):
- Action: ECG/monitoring now; plan oral anticoagulation if indicated when safe (see below) even if imaging looks “lacunar”, may require surgical repair of structural cardiac lesions.
-
~¼ Other/cryptogenic (dissection, thrombophilia, hyperviscosity; higher in young):
- Clues: neck pain/trauma for dissection; hypercoagulable risk factors; migraine-like prodromes with sudden negative deficits.
- ED actions: CTA head/neck to assess dissection/stenosis; short-course (21 days) DAPT for TIA/nondisabling stroke unless cardioembolic mechanism surfaces; coordinate targeted work-up with consultant.
Etiology is not an academic afterthought—it determines secondary prevention timelines, including both medications and interventional procedures. Large-artery atherosclerosis (carotid or intracranial) may require a surgical approach when symptomatic ICA stenosis is present; pre-op therapy is typically single antiplatelet, and the procedural window is early (after the first 48 hours, but ideally within the first couple of weeks). Lacunar or small-vessel disease typically requires an antiplatelet-based prevention strategy with aggressive risk-factor control; thrombolysis is reserved for disabling presentations within the treatment window. Cardioembolic sources (most commonly atrial fibrillation, but also structural heart disease) shift the plan toward oral anticoagulation once it is safe, so an ECG at the time of presentation and arrangements for rhythm monitoring and echocardiography matter even in nondisabling stroke or high risk TIA cases. Cervical artery dissection and other “cryptogenic/other” mechanisms are proportionally more common in younger patients; they necessitate CTA head/neck to confirm the diagnosis and typically lead to a short course of dual antiplatelets for TIA/nondisabling stroke presentations while awaiting confirmatory testing for underlying stroke etiology.
Imaging strategy and timing for nondisabling stroke
The appropriate acute imaging study in suspected ischemic stroke is a stroke-protocol CTA performed immediately, not a delayed “carotid stenosis” CTA intended for elective surgical planning. The stroke-protocol CTA provides time-sensitive information essential to emergency management: identifying the site of occlusion, assessing collateral circulation, and detecting stenosis or dissection that may alter acute therapeutic decisions.
A normal early CT or CTA does not exclude ischemic stroke. Lacunar infarcts, distal vessel occlusions, and small ischemic cores can be radiographically occult in the hyperacute phase. Clinicians should treat the clinical syndrome, and when imaging findings appear discordant with the patient’s presentation, pursue specialist advice rather than prematurely excluding the diagnosis.
Carotid and vertebral Doppler ultrasonography remain useful for secondary prevention and pre-operative assessment, but they do not substitute for CTA when available to inform real-time decisions in the ED.
Carotid endarterectomy (CEA) in nondisabling stroke / high-risk TIA
Carotid endarterectomy remains one of the few surgical interventions in stroke care that meaningfully alters outcomes. Patients with symptomatic internal carotid artery stenosis of 70–99% derive the greatest absolute risk reduction in recurrent stroke with early CEA. Selected patients with 50–69% stenosis may also benefit, depending on plaque/composition/stability, comorbidities, and symptoms.
Timing is critical: CEA is typically deferred for the first 48 hours following ischemic stroke to avoid reperfusion injury in the “hot brain” phase, then performed as soon as safely feasible—ideally within 7–14 days of the index event. The benefit declines substantially with delay beyond two weeks.
Emergency clinician priorities:
- Ensure accurate CTA-based quantification of carotid stenosis.
- Initiate antiplatelet therapy promptly.
- Expedite referral for vascular surgery or stroke specialist evaluation—direct booking of urgent follow-up is often warranted.
- Inititate single-agent antiplatelet therapy promptly (typically aspirin) preoperatively unless dual therapy is specifically recommended by surgical or stroke colleagues.
Medical therapy for nondisabling stroke: Secondary prevention
Once intracranial hemorrhage is ruled out:
High-risk TIA and nondisabling stroke live on the same continuum and should be managed with the same urgency. Load antiplatelets in the ED and tailor the regimen to mechanism. Most patients without endarterectomy plans or atrial fibrillation benefit from a short course of dual antiplatelet therapy (DAPT)—typically 21 days—then de-escalation to monotherapy. Pragmatically, aspirin 160–325 mg loading then 81 mg daily combined with clopidogrel 300 mg loading then 75 mg daily is common; aspirin with ticagrelor 180 mg loading then 90 mg twice daily is a reasonable alternative. Benefit is front-loaded in the first three weeks; bleeding risk rises after, which is why DAPT is not continued indefinitely as a standard. Use single antiplatelet therapy if carotid surgery is anticipated, extend dual antiplatelet therapy when intracranial atherosclerosis is the culprit per local protocol, and/or transition to anticoagulation when cardioembolic sources such as atrial fibrillation are identified and it is safe to do so. For symptomatic cervical artery dissection with TIA or nondisabling stroke, treatment typically involves a short course of DAPT, while asymptomatic dissection commonly receives single-agent therapy for months in coordination with the stroke team.
Landmark stroke dual antiplatelet therapy (DAPT) trials
- THALES (2020): Minor ischemic stroke/high-risk TIA—ASA+ticagrelor reduced 30-day stroke or death versus ASA alone; absolute benefit front-loaded with a small increase in major bleeding. Implication: viable DAPT alternative when clopidogrel resistance/genotype is a concern.
- CHANCE-2 (2021): In CYP2C19 loss-of-function carriers, ticagrelor-ASA lowered 90-day stroke versus clopidogrel-ASA without excess severe bleeding. Implication: supports genotype-guided DAPT choice favoring ticagrelor in LOF carriers.
- INSPIRES (2023): Mild stroke/high-risk TIA—clopidogrel-ASA initiated early (often beyond hyper-acute hours) reduced recurrent stroke vs ASA alone; small increase in major bleeding. Implication: reinforces short-course DAPT even with delayed presentation.
- ARAMIS (2023): Minor nondisabling stroke within thrombolysis window—DAPT non-inferior to IV alteplase for 90-day functional outcomes with lower hemorrhagic risk. Implication: in truly nondisabling cases, optimized DAPT may be reasonable when thrombolysis is unlikely to change function.
Antiplatelet therapy for nondisabling stroke
-
Single antiplatelet medication options:
- Aspirin 160–325 mg load → 81 mg daily, or
- Clopidogrel 300 mg load → 75 mg daily (use when ASA allergy/intolerance or DAPT chosen).
-
DAPT (short course ~21–28 days):
- ASA + clopidogrel (default in many pathways) then step down to single antiplatelet agent.
- Consider ASA + ticagrelor where clopidogrel resistance/genotype is a concern.
- Avoid DAPT in disabling infarcts (higher bleed risk into established core).
-
Etiology-specific nuances:
- Intracranial atherosclerosis: consider DAPT ~90 days.
- Cervical artery dissection: often DAPT ~21 days for TIA/nondisabling stroke; some specialists prefer anticoagulation; asymptomatic dissections frequently single antiplatelet agent ≥6 months.
- Peri-carotid endarectomy: typically single antiplatelet pre-op (confirm with vascular/stroke protocols).
Anticoagulation after nondisabling stroke – The 1-2-3-4-Day Rule
-
Cardioembolic sources (e.g., AF): oral anticoagulation for secondary prevention; initiation/timing individualized (consider infarct size, hemorrhagic risk, and neurology guidance) but typically within 4 days; the trend as of 2025 is to start a DOAC as soon as 24 hrs after the stroke initiation for smaller infarcts with low hemorrhagic transformation risk.
- The “1-2-3-4-Day” rule proposes starting DOACs after ischemic stroke with atrial fibrillation at 1, 2, 3, or 4 days post-event, depending on stroke severity (TIA, mild, moderate, or severe, respectively), and was associated with reduced recurrent stroke or systemic embolism risk without increased major bleeding in both Japanese and European cohorts.
Blood pressure & lipids after nondisabling stroke
- Avoid aggressive BP reduction in the ED (see Part 1 for details); target gradual control.
- Consider starting high-intensity statin (e.g., atorvastatin 80 mg) unless contraindicated.
Lifestyle and risk factor management after nondisabling stroke
-
Smoking cessation, diabetes optimization, physical activity, and diet counselling—all should begin in the ED discharge summary or follow-up instructions.
Disposition decisions for nondisabling stroke
Disposition decisions for patients presenting with acute nondisabling stroke should be individualized, guided by risk stratification and institutional resources. Admission to a specialized stroke unit is associated with improved outcomes even in nondisabling presentations and should be prioritized when high-risk features are present or reliable outpatient follow-up cannot be assured.
Admission Criteria for nondisabling stroke
Hospital admission or observation is recommended for patients with any of the following:
- Symptomatic extracranial or intracranial stenosis >50%
- Acute infarction on MRI
- New-onset atrial fibrillation or other cardioembolic source
- Recurrent (dual) TIAs or crescendo symptoms
- Severe or labile hypertension
- Metabolic derangements or medical instability
- Uncertain diagnosis or unreliable follow-up
- Institutional barriers to rapid outpatient evaluation
Safe discharge criteria for nondisabling stroke (with follow-up ≤48 hours)
Selected patients with nondisabling stroke can be discharged safely from the ED when all of the following are satisfied:
- Mild neurological deficit (NIHSS ≤5)
- Stable neurological symptoms without recurrence, progression, or fluctuation
- Brain imaging (CT/MRI) excludes hemorrhage, large vessel occlusion, or high-risk pathology (e.g., >50% carotid stenosis)
- Lab tests show no significant acute abnormalities (e.g., no atrial fibrillation, troponin elevation, or metabolic derangements)
- Initiation of secondary prevention: antiplatelet/anticoagulation and statin as indicated
- Expedited outpatient follow-up arranged within 24-72 hours with stroke or neurology clinic
Key take home points for nondisabling stroke recognition and management
- Nondisabling strokes account for a substantial proportion of ED cerebrovascular presentations and carry a 4–5% 30-day risk of deterioration or disabling stroke; early recognition, imaging, and secondary prevention remain urgent priorities.
- Roughly 1 in 10 strokes are initially missed, and a similar proportion of presumed strokes are mimics (e.g., vestibular disorders, metabolic, migraine, functional neurologic disorder, hypoglycemia). The cost of missing stroke is far greater than treating a mimic. Distinguish by tempo (abrupt vs. gradual), symptom type (negative vs. positive), distribution (neuroanatomic vs. patchy), and laterality (unilateral vs. bilateral). Always rule out hypoglycemia and perform a gait/truncal ataxia assessment to avoid missing posterior strokes.
- Features of functional neurologic disorder include inconsistency, give-way weakness, and distractibility. However, functional does not mean feigned—up to 60% have underlying organic disease. Never diagnose “functional stroke” without objective testing and neurology consultation; err on the side of treating as stroke until proven otherwise.
- Up to 18% of strokes occur under age 50, often misattributed to migraine, anxiety, or “functional” causes, particularly in women. Maintain suspicion with sudden negative focal deficits and order CTA head/neck when the story fits. Dissection, PFO, and hypercoagulable states are key etiologies.
- A common pitfall is underestimating urgency in nondisabling strokes due to subtle deficits, especially in younger patients and women.
- TIA and nondisabling stroke share the same pathophysiology, prognosis and treatments—13% of TIAs show infarct on MRI, and up to 17% progress to disabling stroke within 90 days, most within 48 hours. Treat both with equal urgency in imaging and antithrombotic initiation.
- Imaging strategies should favor immediate stroke-protocol CTA to identify occlusion, stenosis, or dissection; normal early imaging does not exclude stroke.
- Normal early CT/CTA does not necessarily rule out stroke—lacunar and distal lesions may be initially occult. Treat the clinical syndrome and repeat imaging when data conflict with presentation.
- Secondary prevention includes initiating antiplatelet therapy, statins, and addressing modifiable risk factors; a 21-day course of dual antiplatelet therapy is common.
- Mechanism Dictates Management — The Rule of 4s. Etiology drives therapy:
- ¼ Large-artery atherosclerosis: DAPT or CEA pathway depending on degree of stenosis, single antiplatelet pre-op.
- ¼ Lacunar: DAPT, risk-factor control.
- ¼ Cardioembolic: anticoagulation typically within 4 days, as early as 24hrs.
- ¼ Other/cryptogenic: dissection, thrombophilia, or hypercoagulable states—often DAPT for 21 days – consult stroke specialist.
- Carotid endarterectomy timing is vital—ideally within 7–14 days after ischemic stroke in symptomatic carotid stenosis >70% ≤99% and selected patients >50% ≤69%, with deferred surgery in the first 48 hours.
- Disposition decisions depend on risk stratification; safe discharge requires NIHSS ≤5, stable deficits, no high-risk imaging or lab abnormalities, and guaranteed expedited follow-up.
References









