Podcast: Play in new window | Download
In this main episode podcast, Dr. Arun Sayal creator of the CASTED course and Dr. Yatin Chadha a radiologist with a fellowship in MSK radiology, join Anton for Part 1 of 2 podcasts on Emergency Orthopedic Injuries. This episode focuses on a differential diagnosis of MSK injuries that are occult to X-ray with the help of the SCARED OF mnemonic. It ensures we pick up all the “can’t miss” diagnoses that can be easily overlooked when we do not integrate a pointed history and physical exam with the X-ray in front of us. Essentially, we discuss ‘when X-rays lie’ and offer up a variety of clinical pearls and pitfalls in assessing patients in the ED with MSK presentations…
Podcast production, sound design & editing by Anton Helman; voice editing by Braedon Paul
Written Summary and blog post by Kate Dillon & Ian Beamish, edited by Anton Helman October, 2022
Cite this podcast as: Helman, A. Chadha, Y. Sayal, A. Emergency Orthopedics Differential: SCARED OF Mnemonic. Emergency Medicine Cases. October, 2022. https://emergencymedicinecases.com/orthopedics-differential-scared-of-mnemonic. Accessed October 26, 2022
The occult MSK X-ray: A normal X-ray does not preclude serious pathology
Just as a normal ECG does not rule out ACS, a normal x-ray does not rule out all serious MSK pathology. We tend to over-rely on x-rays to diagnose orthopedic injuries, sometimes overlooking key historical and physical exam data points that should inform our pre-test probability. As in all ED presentations, we should apply Bayesian analysis to orthopedic cases.
Using history to inform our pre-test probability for MSK pathology
Important aspects in history taking for MSK presentations that may influence pre-test probability:
- Age (certain fractures tend to occur in specific age ranges e.g. scaphoid fractures have peak incidence age 20-29)
- Traumatic/atraumatic mechanism
- Previous injuries
- Past medical history (e.g. cancer/autoimmune disease/other immunocompromising disease, osteoporosis)
- Medications (e.g. steroids/immunosuppressants – risk factors for septic arthritis, medications for osteoporosis)
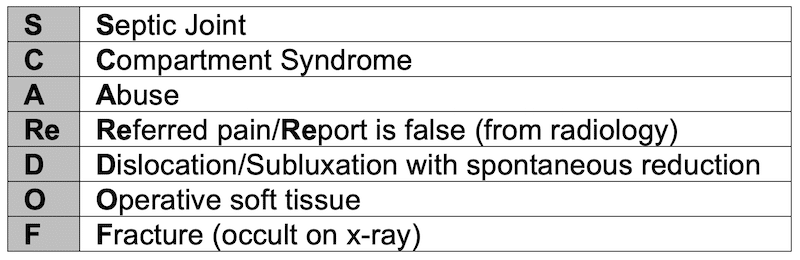
Dr. Sayal’s SCARED OF mnemonic: An approach to orthopedic differential diagnosis
In the presence of a normal (or near-normal) X-ray, what should we be “scared of”?
1. Septic arthritis
For patients who present with non-traumatic MSK pain, infection including septic arthritis/bursitis, osteomyelitis and discitis and should be near the top of the differential diagnosis.
The accuracy (or inaccuracy) of lab tests for septic arthritis
The likelihood ratios for serum tests are variable across studies and do not appear to be very predictive, especially in immunocompromised patients. In one review “no cutoff for ESR or CRP significantly increases or decreases the post-test probability of septic arthritis.”
- ESR > 20mm/hr +LR 0.84, -LR 2.4
- ESR > 30mm/hr +LR 1.3, -LR 0.17
- ESR > 50mm/hr +LR 1.4, -LR 0.4
- ESR >100mm/hr +LR 7.0, -LR 0.6
- CRP >10 mg/L +LR 1.1-1.4, -LR 0.3-0.6
- CRP >100mg/L +LR 1.1-2.8, -LR 0.3-0.6
Synovial fluid tests likelihood ratios
Without testing synovial lactate levels, synovial fluid analysis had an overall sensitivity of only 70-80% which drops to 50% when antibiotics are administered prior to the arthocentesis. However when synovial lactate is included, synovial fluid analysis has excellent test characteristics for the diagnosis of septic arthritis. Tissue culture is the gold standard diagnostic test for septic arthritis.
Synovial PMNs >90% +LR 2.7, -LR 0.51
Synovial lactate >5.6 mmol/L +LR 2.4, -LR 0.46
Synovial lactate >12 mmol/L +LR 19, -LR 0.16
Pearl: Synovial fluid lactate has demonstrated excellent diagnostic accuracy for septic arthritis with +LRs as high as 19 and -LR as low as 0.16.
Pitfall: Synovial fluid analysis overall has a 70-80% sensitivity and antibiotics prior to the tap can drop sensitivity by up to 50%!
In patients with septic arthritis, while some large joints such as the knee often are visibly swollen and relatively easy to access for fluid aspiration, other large joints such as the hip rarely appear visibly swollen, usually require fluoroscopy-guided aspiration and so imaging may be more often used to help support a diagnosis of septic arthritis.
Septic arthritis of the hip is a particularly challenging ED diagnosis: Physical exam pearls and the role of imaging
Physical exam findings of septic arthritis of the hip
- Externally rotated and flexed hip: increases capsule volume, provides patient relief from inflammation/swelling
- Non-weight bearing status is a strong predictor of septic arthritis of a lower extremity joint
- Pain significantly aggravated by ROM: pressure increases in the capsule leading to pain; most patients with septic arthritis have very limited ROM due to pain
Pearl: A patient who presents with non-traumatic hip pain who is lying supine in the stretcher with their hip externally rotated and slightly flexed should raise the suspicion for septic arthritis of the hip.
X-ray findings in septic arthritis: Often overlooked, and if present should increase suspicion
While the x-ray is usually normal in patients with septic arthritis (especially in early presenters), the following findings should increase one’s suspicion for septic arthritis.
- Effacement of fat planes lateral to the hip joint: lateral to the hip joint there are 3 bands of soft tissue (rectus femoris, gluteus minimus and gluteus medius); effacement of the low density strips in between these bands of soft tissue compared to the contralateral side suggest a joint effusion which increases the likelihood of septic arthritis in a patient with non-traumatic hip pain
- Joint space narrowing: joint space narrowing compared to the contralateral side and compared to previous imaging when available
- Bony erosions

Septic arthritis x-ray showing right hip joint space narrowing, bony erosion. Case courtesy of Dr Matt Skalski, Radiopaedia.org. From the case rID: 29079
Ultrasound, CT and MRI in the diagnosis of septic arthritis
- While a joint effusion found on ultrasound increases the likelihood of septic arthritis in patients where you have a suspicion, a negative ultrasound for effusion does not rule out septic arthritis.
- Although CT is generally very accurate at detecting fractures that are occult to x-ray, they are inaccurate for the diagnosis of septic arthritis, and are not the preferred advanced imaging modality of choice according to our experts.
- MRI is the advanced imaging modality of choice for patients suspected of septic arthritis in whom a joint aspiration is not possible or unsuccessful.
Pitfall: A common pitfall is to rule out septic arthritis of the hip if an ultrasound is negative for joint effusion. A negative ultrasound for effusion does not rule out septic arthritis: because the ultrasound of the hip is performed on a supine patient, and fluid collects in the dependent portion of the joint, an effusion may not be seen when evaluating the hip anteriorly.
2. Compartment Syndrome: Forget about the 6 Ps (except for board exams) and yes, it can occur after trauma without fracture
Compartment syndrome clinical clues
Pain out of proportion is usually the first clue to compartment syndrome and patients will rarely have developed any of the other classic 6Ps (Pain, Paresthesias, Paralysis, Pulselessness, Pallor, Poikilothermia) when they present to the ED. When multiple Ps are present it is often too late to salvage the limb.
- Risk factors: there is a higher incidence of compartment syndrome in young, fit males as they have less soft tissue compliance and greater muscle bulk so smaller increases in compartment volume can lead to larger pressure changes
- Mechanisms of injury: in addition to fractures, consider mechanisms such as high pressure injection, tight casts or dressings, soft tissue injuries, burns, extravasation of IV fluids, ‘found down’, and even open fractures
- Palpate the unaffected side to compare the compartments
Pitfall: A common pitfall is to not consider compartment syndrome in patients who sustain an MSK injury without a fracture; do not rely on the presence of a fracture to suspect the possibility of a compartment syndrome; 70% of the cases of compartment syndrome involve a fracture, 30% do not.
Pearl: Make palpating compartments part of your routine neurovascular status exam for orthopedic injuries to improve your ability to pick up an abnormal compartment on palpation
Pitfall: Do not dismiss the possibility of compartment syndrome when pain is the only finding; of the 6 Ps, all except pain are typically not present when patients initially present to the ED. If one of the Ps is present besides pain, it is usually paresthesias.
The role of imaging in compartment syndrome is limited, especially in the acute setting
Acute compartment syndrome is a clinical diagnosis and if the pre-test probability is high on initial assessment, do not allow imaging to delay consultation with orthopedics. CT may show expansion of soft tissue and effacement of fat planes but is not diagnostic and may be misleading.
Compartment pressure measurements should be reserved for comatose patients and/or those in whom a reliable history and physical exam is not possible
Compartment pressures are technically difficult to perform and the traditional cutoff value of >30mmHg is inaccurate for the diagnosis of compartment syndrome. Some have suggested that a delta pressure (diastolic pressure – compartment pressure of <30mmHg may improve accuracy but is still fraught with variability.
Pitfall: Relying on compartment pressure measurement to diagnose compartment syndrome is a pitfall; measurement of compartment pressure should not be a prerequisite for consulting orthopedic surgery for a suspected compartment syndrome.
Deep Dive: EM Quick Hits 9: Clinical Diagnosis Pitfalls of Compartment Syndrome
3. Abuse: X-ray findings consistent with non-accidental injury (NAI)
Although certain fracture patterns have a higher specificity for NAI and should raise your suspicion, none are specific enough to rule in NAI. Multiple fractures at different stages of healing are highly suspicious for NAI.
Fractures with high specificity for NAI in pediatric population
1.Pediatric metaphyseal corner fracture: usually subtle, small avulsion fracture at the corner of the metaphysis, typically seen in long bones (proximal tibia/distal femur, proximal humerus), multiple or bilateral findings should raise suspicion further.

Pediatric metaphyseal corner fracture. Source: Case courtesy of Dr Hani Makky Al Salam, Radiopaedia.org, rID: 13614
2.Pediatric posterior rib fracture: mechanism is a squeezing injury of the chest, difficult to visualize acutely on X-ray due to overlap of transverse processes and posterior ribs (fractures are often just lateral to this area), becomes more apparent when healing starts to occur

Healing pediatric posterior rib fractures. Source: Wikipedia
3.Unusual location fractures: acromion, sternum and spinous process are unusual in pediatric population
Lower specificity fractures for NAI: eggshell pattern of the skull (multiple fractures), impacted occiput fracture, adult radius spiral fracture from forceful twisting of the forearm
Deep Dive: Episode 108: Pediatric Physical Abuse Recognition and Management
4. Referred pain: The importance of a good clinical exam
Referred Pain – often more proximal source
Common Areas of Referred Pain:
- Hip Pain presenting as knee pain:
- Slipped capito-femoral epiphysis (SCFE): pediatric patient presenting with knee pain
- Hip fracture: elderly population, medial knee pain
- Elbow pain or shoulder pain originating from the neck
Clinical Pearl: examine the joint above and below the point of maximal pain; example – examine the hip (with internal/external rotation) of all older patients presenting with medial knee pain; although chronic OA pain may limit hip ROM, a hip fracture should be considered.
5. Report is False: Top 9 MSK X-ray misses
The miss rate for plain films in EDs is about 5%
- 1% of these misses are an “overcall” on the 80% of “nil acute plain films”
- 4% of these misses are a “miss” on the 20% of films that show pathology; i.e. 20% of pathology being missed
Commonly missed fracture sites by age
- Pediatrics – elbow, wrist, and foot
- Adults – foot and hand
- Older people – pelvis and hip
Commonly missed injuries include:
1.Posterior shoulder dislocation
2.Pediatric lateral condyle fracture: linear flake avulsion off the lateral aspect of the distal humerus

Image Source: https://elentra.healthsci.queensu.ca/assets/modules/ts-ped-elbow-radiograph/Picture23.png
3.Coronoid process fracture: mechanism of posterior dislocation, small fragment off the tip of the coronoid process

Image Source: Case courtesy of Dr Mohamed Mahmoud Elthokapy, Radiopaedia.org rID: 97518
4.Distal radio/ulnar joint dislocation/DRUJ subluxation: widened distal radioulnar joint space on AP view, and dorsal or volar displacement on the lateral view

Distal radio/ulnar joint dislocation/DRUJ subluxation: widened distal radioulnar joint space on AP view, and dorsal displacement of distal ulna on the lateral view. Source: https://els-jbs-prod-cdn.jbs.elsevierhealth.com/cms/attachment/f241dfc9-ac69-4d21-a96f-cce7edf4bca3/gr1_lrg.jpg
5.ACL Tear: indentation/impaction of femoral condyle >2mm on the lateral view with joint effusion suggests an ACL tear

Femoral condyl impaction type fracture. Image Source: https://www.orthobullets.com/knee-and-sports/3008/acl-tear
7.Ankle subluxation/instability:
- Mortise asymmetry – on the mortise view asses for symmetry of the ankle joint space (mortise); asymmetry or joint space widening >4mm suggests subluxation/instability

Ankle mortise asymmetry suggesting instability. Source: Case courtesy of The Radswiki, Radiopaedia.org, rID: 11592
- Distal tibial-fibular syndesmosis clear space and overlap – widening of the clear space between the medial border of the fibula and the lateral border of the posterior tibia ≥6mm on AP view and/or overlap of the fibula and the anterior tibial tubercle >6mm on the AP view, >1mm on the mortise view suggests ankle instability

Clear space and overlap on AP view ankle. Source: Tessa Davis . Ankle x-rays, Don’t Forget the Bubbles, 2016. Available at: https://doi.org/10.31440/DFTB.9992
8.Pediatric elbow subluxation/dislocation: a radiocapitellar line that does not bisect the middle 1/3rd of the capitellum suggests elbow subluxation or dislocation +/- occult fracture

Radiocapitellar line in normal elbow x-ray.Source: Case courtesy of Dr Samir Benoudina, Radiopaedia.org, rID: 41196
9.Carpometacarpal subluxation/dislocation: bases of 4th and 5th metacarpals normally do not significantly overlap with the hamate on the AP view. A large degree of bony overlap suggests subluxation or dislocation.

Anterior dislocation of base of 5th metacarpal. The 5th CMC joint space should normally be seen on the AP as a thin space between the metacarpal base and the hamate, or a slight overlap of the bones. A large degree of bony overlap suggests subluxation or dislocation. Source: Case courtesy of Dr Thuan Tzen, Koh, Radiopaedia.org, rID: 34851
6.Dislocation/Subluxation has been reduced
Knee Dislocation: potentially limb threatening, these may reduce in the field, and present as a swollen tender knee in the ED
Rare diagnosis but consider in:
- High energy injury (MVC, high injury sports)
- Patients with high BMI and/or older patients
Examine the contralateral side for comparison.
Assess stability of the knee (Lachman and valgus/varus); 3 ligament instability suggests knee dislocation.
Deep Dive: Episode 91: Occult Knee Injuries Pearls and Pitfalls
7.Operative soft tissue injury: Which injuries can’t wait?
Soft tissue injuries that usually require urgent orthopedic consultation and surgery as delay in diagnosis may lead to poorer outcomes:
- Acute Complete Rotator Cuff Tear (middle-aged patients 40s-50s)
- Quadriceps Tear
- Patellar Tendon Tear
- Distal Biceps Rupture
- Achilles Tendon Rupture (may be managed non-operatively)
- Locked Knee from Meniscal Tear
Deep Dive: Episode 58: Tendons and Ligaments: Commonly Missed Uncommon Injuries Part 2
Episode 121: Elbow Injuries – Ten Pitfalls in Diagnosis and Management
8.Fracture (Occult): Use your pre-test probability as your guide
Use your pre-test probability based on history and physical to inform your concern for fracture in the context of a “normal” X-ray. If their is a high clinical suspicion for fracture in patients with normal X-rays consider immobilization and followup with orthopedics or advanced imaging if delay to surgery is a concern (e.g. hip fracture). Some common occult fractures to X-ray include: scaphoid, pediatric growth plate fractures, stress fractures, hip fractures and c-spine fractures.









