פוסט זה זמין גם ב:
עברית
Written by Davin Brar
Spoon Feed
Among patients with symptomatic PE who are low risk by sPESI, the addition of right ventricular assessment predictors (echo, CT, troponin, and BNP) significantly improved prognostication for clinical deterioration within 5 days.
Why does this matter?
Appropriate disposition for patients diagnosed with pulmonary embolism (PE) is both extremely important and exceedingly challenging. Even when using scoring criteria such as sPESI or HESTIA, emergency physicians are often hesitant to discharge “low risk” patients. The objective of this study was to assess if markers of right ventricular (RV) dysfunction in low-risk patients could provide better prognostication of patients who are at high risk of morbidity within 5 days. This could help to further risk stratify patients with PE and provide additional information to guide management and disposition.
PE + RV assessment = home?
This was a prospective, observational study using a PE registry database from 6 academic EDs in the US. The study included patients with acute symptomatic PE who were considered low risk by sPESI (score of 0). Using imaging (goal directed echo & CT angiography) and cardiac biomarkers (troponin and BNP), the authors used a prediction model to assess whether RV assessment could improve prognostication of low-risk PE patients who suffered from clinical deterioration (CD) within 5 days. CD was defined as death, respiratory failure, cardiac arrest, dysrhythmias, sustained hypotension, or escalated PE intervention.
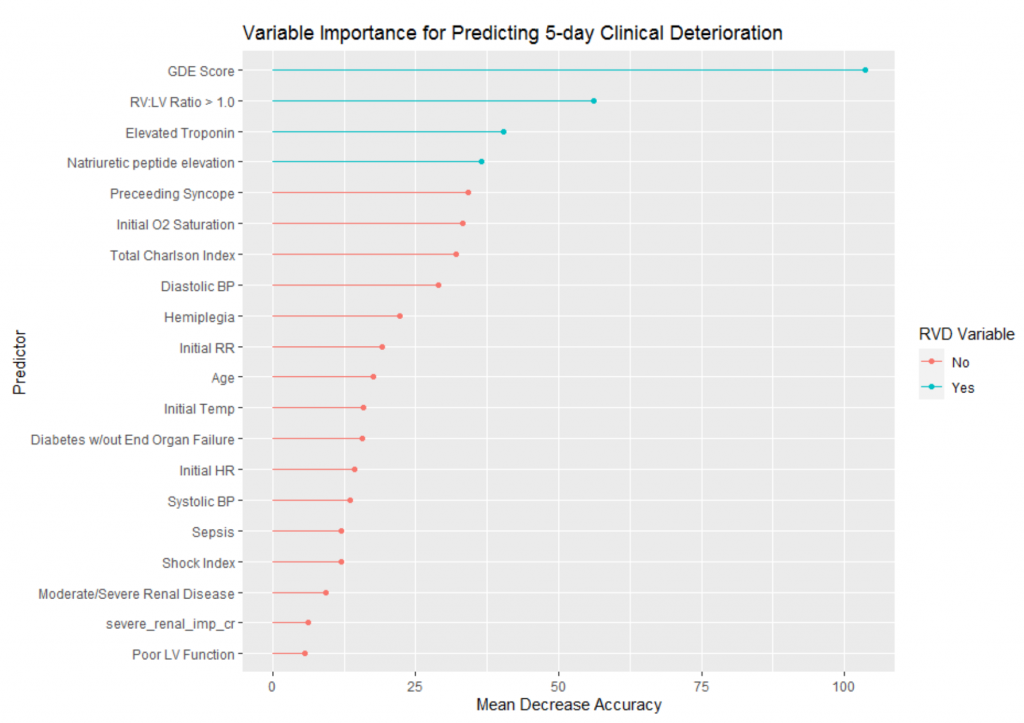
There were 610 low-risk PE patients with sPESI = 0, of which 11.8% (72) had CD within 5 days. RV abnormalities were identified in 26% of low-risk patients by CT, 20% by echo, 22% by BNP, and 18% by troponin. Using a random forest model, the authors determined that the top four predictors for CD within 5 days were the four RV assessment predictors (CT, echo, BNP, troponin), with echo being the most important factor. See figure.
Furthermore, 90% of low risk people who suffered CD would have been correctly reclassified as higher risk if tools incorporating RV dysfunction were used (like the PE-SCORE). Some limitations of this study included a relatively small sample size, the fact that these EDs admitted all patients with RV abnormalities, and that all echocardiograms were POCUS but were reviewed and documented by a trained quality assurance provider.
This study gives us more information on how to appropriately risk stratify patients with PE. Not every “low risk” PE patient by sPESI is safe for outpatient treatment, and it is important to consider RV abnormalities (especially bedside echo) and other factors such as the ability to follow up, medication adherence, bleeding risk, etc. when determining the appropriate management and disposition.
Edited and Peer-Reviewed by Sam Parnell and Nick Zelt
Source
Can right ventricular assessments improve triaging of low risk pulmonary embolism? Acad Emerg Med. 2022 Mar 15. doi: 10.1111/acem.14484. Online ahead of print.








