פוסט זה זמין גם ב:
עברית
Podcast: Play in new window | Download
“This learning material is sourced from Emergency Medicine Cases and has been published here with permission as per creative commons copyright”
EM Quick Hits 54 Button Battery Ingestion, C. difficile, ECG in Tox, Bed Bugs, Fibrinogen in Trauma, Cold Air for Croup
Topics in this EM Quick Hits podcast
Olivia Ostrow on the management of pediatric button battery ingestions and impaction (1:15)
Brit Long on c. difficile infection (19:15)
Jesse McLaren on an approach to ECGs in the poisoned patient (26:34)
Joe Mullally on the identification and treatment of bed bug bites (31:50)
Andrew Petrosoniak on fibrinogen replacement in bleeding trauma patients (38:30)
Justin Morganstern on cold air for management of croup (48:35)
Written summary & blog post by Shaila Gunn and Brit Long, edited by Anton Helman
Cite this podcast as: Helman, A. Ostrow, O. Long, B. McLaren, J. Mullally, J. Petrosoniak, A. Morgenstern J. EM Quick Hits 54 – Button Battery Ingestion, C. difficile, ECG in Tox, Bed Bugs, Fibrinogen in Trauma, Cold Air for Croup. Emergency Medicine Cases. January, 2024. https://emergencymedicinecases.com/em-quick-hits-january-2024/. Accessed January 24, 2024.
Button battery ingestion and impaction

Button battery ingestion with esophageal impaction is a potentially life-threatening emergency with damage to tissues typically starting within minutes-hours, but may be delayed by weeks-months. More than 50% of serious outcomes due to button battery ingestion occur after unwitnessed ingestions, in which case there is likely a delay in recognition and management.
- How is the tissue damaged? The tissue injury is a caustic chemical reaction (rather than thermal) – this leads to an alkaline burn and liquefactive necrosis through the esophagus, trachea, and major blood vessels which may lead to severe complications including tracheoesophageal and aortoesophageal fistulas.
- Location of impaction matters: Impactions in the proximal and mid esophagus are most dangerous. The risk of injury decreases if it is lodged in the stomach or duodenum.
- Timing of tissue damage/symptoms/complications: Coagulative necrosis has been shown to start within 15 minutes of contact but complications may be delayed up to 2 months. Symptoms may take hours to days to develop but the damage to tissues occurs within 2 hours making suspicion for button battery ingestion and prompt recognition important. If the button battery is removed within a 2 hour time frame, the risk of severe and fatal injury decreases significantly. The risk of perforation increases dramatically after 12 hours. Parents must continue to monitor for symptoms of tissue damage even if the button battery was removed.
- What type of battery? Serious complications and death from button battery ingestion are associated most frequently with 3V lithium batteries ≥20mm.
- If a parent thinks the child swallowed a coin – assume button battery ingestion until proven otherwise.
- Presenting symptoms may be subtle and nonspecific: classic findings of foreign body ingestion (i.e. cough, chest pain, wheeze), vomiting, hematemesis, poor feeding/food refusal or fever.
ED management of button battery ingestion
- Administer a neutralizing agent
- Sucralfate, (or pasteurized honey if sucralfate is unavailable), should be given immediately, so long as it does not cause a delay in removal of the battery, it is given within 12 hours of ingestion and there are no airway concerns. Both work by reducing pH and coating the battery to delay alkaline burns to tissue.
- Dosing honey for management of button battery ingestion: 2 teaspoons (10 ml) of honey every 10 minutes up to 6 doses OR
- Dosing sucralfate for management of button battery ingestion: sucralfate 1g (10 ml) every 10 minutes up to 3 doses
- STAT AP and lateral x-ray of the neck and chest to localize the battery
- The Halo and Step-off Signs on AP & Lateral X-ray are pathognomonic of a button battery and help distinguish a button battery from a coin or other round FB.
- Halo sign: seen on AP as a ring within a ring (zoom in on the area of concern)
- The Halo and Step-off Signs on AP & Lateral X-ray are pathognomonic of a button battery and help distinguish a button battery from a coin or other round FB.
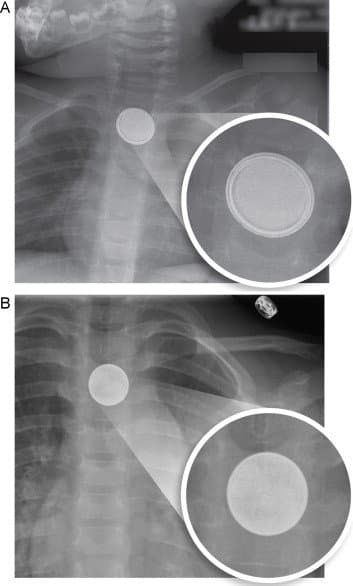
Top image (A) showing double circle halo sign in keeping with impacted button battery vs bottom image (B) showing single circle in keeping with impacted coin on AP chest x-ray
-
-
- Step-off sign: seen on lateral
-
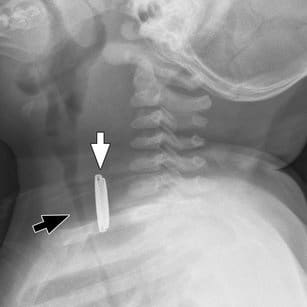
Step-off sign of impacted button battery on lateral x-ray of the neck
Management of button batteries found in the stomach or colon
A controversial area in the management of button battery ingestions is in the asymptomatic patient with a battery found distal to the esophagus the esophagus (eg, intragastric, duodenal, and so forth). Recent expert opinion-based guidelines from the Endoscopy Committee of the North American Society for Pediatric Gastroenterology, Hepatology, and Nutrition (NASPGHAN) recommended consideration of endoscopic assessment and removal in:
- patients <5 year old OR
- the battery is > 20 mm in diameter
Prevention of button battery ingestions
- Public engagement and knowledge translation is critical to informing parents/guardians of the dangers of button battery ingestion.
- Counselling families with young children about how to safely use, store, and discard of batteries can help to prevent devastating injuries.
- Simple tips such as storing batteries out of reach and sight, taping over battery compartments, and recycling used batteries can help to reduce the risk of unintentional ingestion.
C difficile infection – what ED docs need to know
Clostridioides difficile is an anaerobic Gram-positive, spore-forming, enterotoxin-producing bacterium that causes watery diarrhea. About 10% of patients presenting to the ED with diarrhea have c difficile infection (CDI).
Risk factors for CDI may include:
- Antibiotic use: Fluoroquinolones, beta-lactam and beta-lactamase inhibitors, third- and fourth-generation cephalosporins, carbapenems, and clindamycin. Even a single dose can cause c diff.
- Health care exposure.
- Patient health factors including inflammatory bowel disease, HIV, recent GI surgery, tube feedings, malnutrition, obesity, female sex, low albumin, and older age.
- PPI use is also considered a risk factor, but this is controversial due to poor data.
- Up to 40% of patients with CDI don’t have a prior antibiotic risk factor, and up to 18% have no prior healthcare exposure.
Suspect CDI in the following patient presentations:
- Ill-appearing patient with diffuse, watery stools and recent antibiotic use and/or hospitalization.
- Abdominal pain (6-90%), fever (21-50%), bloody stools (5-21%) and watery diarrhea (55-84%). Diarrhea is often not an isolated symptom; nausea and vomiting can occur in up to 30%.
- Patients with acute onset of 3 or more unformed stools without explanation.
- Patients with GI symptoms plus constitutional symptoms, as well as a pertinent history of antibiotic use, comorbid conditions, and/or recent healthcare visits.
CDI testing centers on detection of the organism itself or the production of toxin A or B. Culture is not as feasible in the ED. The most common tests in the ED include toxin assay and nucleic acid amplification.
- Toxin assay is specific but has a sensitivity of only 50%-60%.
- NAAT is very sensitive, but it can’t distinguish infection from asymptomatic colonization, so only order the test if the patient has symptoms.
- IDSA guidelines emphasize using a two or three step algorithm based on laboratory capabilities and institution.
Treatment of c. difficile diarrhea depends on illness severity:
- Non-severe
- First episode: vancomycin 125 mg 4x per day for 10 days or fidaxomicin 200 mg 2x per day for 10 days. If these aren’t available, use metronidazole 500 mg 3x per day.
- Severe CDI includes WBC > 15,000 or creatinine > 1.5 mg/dl.
- Use vancomycin or fidaxomicin as above.
- Fulminant CDI includes signs of shock, vasopressor requirement, elevated lactate, or toxic megacolon (peritonitis, severe pain or tenderness, distension, and guarding. Imaging will show a significantly dilated diameter of the colon > 6 cm).
- Speak with GI and surgery early and use enteral vancomycin 500 mg 4x per day. This can be given orally and rectally. If ileus is present use vancomycin rectally.
- Recurrent infection is defined by 3 or more CDI episodes.
- If previously treated with oral metronidazole should be treated with oral vancomycin or fidaxomicin.
- Prevent the spread by washing hands with soap and water with these patients; the alcohol-based sanitizer does not kill the spores.
An approach to ECG’s in the poisoned patient: The tox ECG
¼ of referrals to poison centers provided inaccurate clinically significant/management altering ECG interpretation
See ECG Cases 47 for a detailed dive with examples.
Systematic approach to the tox ECG
- Heart rate and rhythm
- Bradycardia or junction rhythm
- Consider CCB, B-blockers, or digoxin toxicity.
- Tachycardia
- Consider sympathomimetics, anticholinergics, drugs causing vasodilation.
- Sinus tachycardia
- May be hard to identify p-waves if there is a wide QRS or a long QT. Leads II and V1 are the best leads to identify p waves.
- Non-sinus arrythmias and ectopy
- May indicate a more severe toxicity
- Bradycardia or junction rhythm
- Electrical conduction
- PR interval (AV block)
- Consider CCB, B-blockers, or digoxin toxicity.
- QRS duration
- Na channel blockade prolongs QRS.
- QRS>100 is an indication for sodium bicarb.
- QT interval
- K channel blockade prolong the QT.
- QTc > 500 ms is an indication for Mg.
- PR interval (AV block)
- Axis
- Look for rightward axis shift. Na channel blockade has a more profound affect of the right side of the conduction system causing a deep S wave in lead I and a tall R wave in aVR
- ST segment and T-wave changes
- Na channel blockers can cause a Brugada pattern.
- Osborne waves from hypothermia.
- Vasospasm or acute coronary occlusion from cocaine.
- ST depression may be from demand ischemia, hyperkalemia from toxin-mediated vomiting, or be a digitalis effect.
Bed Bugs recognition and management
How to identify bed bugs from other bugs and bites
- Zig-zag pattern (breakfast, lunch, dinner)

Zig zag pattern of bed bug bites
- Pruritic rash
- Bed bug excrements look like black dots
- Bugs look brown, flat, round

Principles of treatment include:
- Usually the rash is self-limiting; manage secondary phenomena. The protein in the saliva can cause an allergic reaction. Bed bugs also serve as a vector for other human pathogens which increase risk of secondary bacterial infections. There is also a significant psychological impact of infestation.
- Preventing infestation in household: Bedbugs can survive 70 days without a meal. Consider vacuuming, steam cleaning, washing sheets at at least 60 degrees Celsius, or hiring an exterminator.
- Medications: A single dose Ivermectin 0.2mg/kg may decrease the population size and number of bites.
Deep dive on bed bugs at Don’t Forget the Bubbles
Fibrinogen replacement in bleeding trauma patients – CRYOSTAT2 Trial
Early and Empirical High-Dose Cryoprecipitate for Hemorrhage After Traumatic Injury: The CRYOSTAT-2 Randomized Clinical Trial by Davenport et al.
P: Injured adults requiring activation of the hospitals major hemorrhage protocol with evidence of acute hemorrhage, systolic blood pressure <90 mmHg at any time, and receiving at least 1U of a blood component transfusion.
I: Empiric cryoprecipitate (6 g fibrinogen equivalent) within 3 hours of injury.
C: Usual practice in MTP (waiting for level and giving if level low).
O: The addition of early, empirical, high dose, cryoprecipitate did NOT improve all-cause 28 day mortality.
- What you need to know about fibrinogen and clotting:
- It is a protein made in the liver that helps with platelet aggregation to form strong, stable clots.
- It is the coagulation level affected most and earliest in trauma patients.
- Bleeding patients with low fibrinogen have more blood loss, require more blood products, have worse outcomes, and is associated with increased mortality.
- If low fibrinogen is associated with poor outcomes, then replacing it is good. How to replace fibrinogen:
- We do not have RCT level evidence that in patients with low fibrinogen, replacing it leads to better outcomes. The above statement is an assumption.
- Fibrinogen concentrate (4g fibrinogen) is non-inferior to cryoprecipitate (in cardiac patients) and has some benefits: it is rapidly reconstituted, has a long shelf life, and a low transfusion risk.
- Indications for fibrinogen in the bleeding trauma patient?
- Not empirically for all bleeding trauma patients as not all patients who are severely injured have low fibrinogen.
- If serum fibrinogen level <1.5 g/L – give 4g fibrinogen concentrate.
- Our expert considers fibrinogen administration if +++ bleeding and giving lots of blood products.
Bottom line => Though fibrinogen is affected early in most bleeding trauma patients and low fibrinogen results in greater blood loss, not all severely injured patients have low fibrinogen. Empiric fibrinogen has not been shown to be especially beneficial. The current recommendation is to treat to target serum fibrinogen level >1.5 g/L.
EBM Quick Hits – Outdoor cold air for croup
Study: Outdoor Cold Air vs Room Temperature Exposure for Croup Symptoms: A Randomized Controlled Trial by Siebert et al.
P: 118 children aged 3 months – 10 years. with mild to moderate croup who did not need epinephrine. Everyone got 0.6 mg/kg dexamethasone.
I: Sit outside for 30 minutes if temperature <10 degrees C (Average temperature 5 degrees C.)
C: Sit inside the waiting room
O: Primary outcome was a decrease in Wesley Croup Score (WCS) by 2 or more points. 49% of the cold air group had a decrease in WCS of 2 points or greater compared to 24% of the indoor group. The difference disappeared by 60 minutes.
3 key points EBM from this study
- RCTs often neglect to report harms of treatments.
- Be cautious of surrogate outcomes which are subject to confounding in a way patient-oriented outcomes are not.
- Open label/unblinded trials may be problematic.