Podcast: Play in new window | Download
“This learning material is sourced from Emergency Medicine Cases and has been published
here with permission as per creative commons copyright”
In this part 2 of our 2-part podcast series on dental emergencies we cover traumatic dental emergencies. Dental trauma is common and often associated with facial trauma. In this episode Dr. Chris Nash and Dr. Richard Ngo answer questions like: At what age is it safe to attempt reimplantation of an avulsed tooth in the ED? What are the 3 most time-sensitive dental trauma emergencies? When is Panorex X-ray or CT indicated in dental trauma? What is the preferred solution to transport an avulsed tooth in? What are 3 dental splinting methods we should consider for dental subluxations and avulsions? How should we handle an avulsed tooth to maximize the chances of a successful reimplantation? When are antibiotics indicated after dental trauma? What role does chlorhexidine rinses play in preventing infection after dental trauma? What are the recommended first and second line treatments for persistent dental hemorrhage? and many more…
Podcast production, sound design & editing by Anton Helman; voice editing by Braedon Paul; background research by Ronak Saluja & Ryan O’Reilly
Written Summary and blog post by Anton Helman August, 2023
Cite this podcast as: Helman, A. Ngo, R. Nash, C. Traumatic Dental Emergencies. Emergency Medicine Cases. August, 2023. https://emergencymedicinecases.com/traumatic-dental-emergencies. Accessed September 14, 2023
Basic dental anatomy required for dental trauma emergencies
Dental structures (superficial to deep) to know for dental trauma are enamel, dentin, pulp, alveolar bone:

Care of ALiEM Smiler series
Primary dentition vs permanent dentition
Adults most commonly have 32 teeth (permanent dentition) divided into 4 quadrants: left and right mandibular dentition and maxillary dentition.

Care of ALiEM Smiler series
Children most commonly have 20 primary teeth, usually present by the age of 3 which gradually are replaced by permanent teeth usually between the ages of 6 and 12.
- For children between the ages of 3 and 6 who suffer a tooth avulsion, reimplantation should not be attempted.
- For children between the ages of 7 and 12 who suffer a tooth avulsion, consult a dentist or oral surgeon for decision making around reimplantation, as it is difficult clinically to distinguish primary vs permanent teeth.
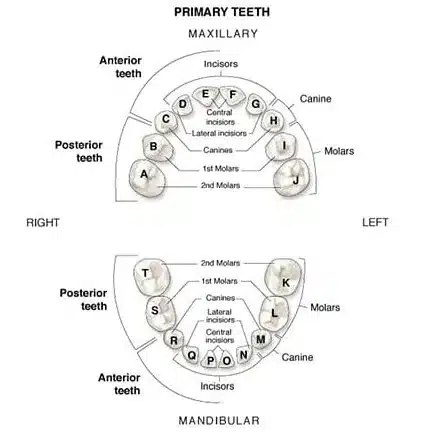
Pitfall: One pitfall is to attempt reimplantation of a primary tooth that has been avulsed. This may lead to ankylosis and prevention of permanent tooth eruption.
Categories of dental trauma: fractures, subluxations, intrusions and avulsions
Dental fractures – uncomplicated vs complicated
The most common traumatic dental injuries are uncomplicated fractures of the enamel and/or dentin of crown of the tooth (do not extend to level of pulp) which require only observation and follow up with outpatient dentist for consideration of re-bonding. Re-bonding can be attempted in the ED.
Complicated dental fractures involve the pulp of the tooth resulting in exposure of the dental pulp to the oral cavity. Patients often experience severe pain and tooth sensitivity and will ultimately require either a root canal or tooth extraction as an outpatient to prevent infection. In the ED calcium hydroxide should be applied to the exposed pulp that is clearly seen as pink tissue within the tooth and arrangements for follow-up with a dentist should be made within 7 days.
Subluxations/Avulsions
Tooth subluxations should be treated with a dental splint (see below) for at least 2 weeks.
Tooth avulsions should be re-implanted and splinted (see below) ASAP in the ED whenever possible.
True traumatic dental emergencies
The most time sensitive traumatic dental emergencies include:
- Complicated dental fractures involving the pulp of the tooth (requires cap of exposed pulp in ED)
- Tooth intrusions >3mm +/- underlying alveolar bone fracture (requires repositioning and stabilization in the ED)
- Tooth avulsions (requires reimplantation, when possible, in the ED)
Imaging in traumatic dental emergencies – indications, Panorex vs CT
Consider a CXR to identify aspirated tooth fragments or whole tooth if these cannot be accounted for otherwise.
Panoramic x-ray (‘Panorex’ view) is indicated for all dental trauma according to the International Association of Dental Traumatology, however, the practical use of this x-ray in the ED is to rule out alveolar bone fracture, mandible or maxillary fractures when CT is not available or contra-indicated.

Panorex view showing right undisplaced mandible fracture
Pre- and post-procedural imaging is important to ensure improved positioning after a dental fracture, subluxation or intrusion has been reduced.
CT is generally reserved for suspected mandibular or maxillary fractures and are usually not helpful for isolated tooth fractures.
Mandible fracture should be suspected if the patient is unable to open their mouth >5cm and/or has a positive tongue blade bite test)
Pitfall: one common pitfall is the failure to consider an aspirated tooth or tooth fragment. If not all teeth/tooth fragments can be accounted for, obtain a CXR to rule out an aspirated tooth or tooth fragment.
Principles of ED dental trauma management
- Dental trauma is often associated with other facial trauma; be sure to assess for non-dental facial trauma, including mandibular fracture, maxillary fracture etc in all patients with trauma to the teeth.
- A mobile tooth suggests either a root fracture or subluxation and should be splinted in the ED.
- For dental fractures with an associated suspected alveolar (bone) fracture (the ridge of the tooth), consider consultation with an oral surgeon in the ED.
- Dental fractures with visible exposed pulp should be treated by capping (covering the exposed pulp) with calcium hydroxide in the ED.
- Milk is preferred over saline to submerge an avulsed tooth in for transport of the tooth.
- The time that a tooth is avulsed is inversely proportional to the chances of reintegration of the tooth after reimplantation; time is tooth!
- Do not attempt reimplantation of a complicated crown fracture, fractured root or dental injury with alveolar fracture.
- Factors to increase the suspicion for non-accidental dental trauma include lip laceration or bruising, frenulum tear or tongue laceration in a non-ambulatory infant, missing or fractured teeth and/or mandible or maxillary fracture with an implausible mechanism of injury.
Pain management for dental emergencies including dental nerve blocks
For dental trauma in which the pulp is exposed, pain can be treated quickly and effectively with a calcium hydroxide cap application or surgical skin glue application (eg. Dermabond, Swiftset). Otherwise, for mild to moderate pain, acetaminophen and NSAIDs are recommended. For severe pain, whenever possible, avoid opioids or prescribed in short courses only in patients with low risk of dependence.
Consider a supraperiosteal nerve block for temporary relief of severe maxillary dental pain:
Consider an inferior alveolar nerve block for temporary relief of severe mandibular dental pain:
Management of dental avulsions and subluxations
For tooth avulsions >20 mins from the time of injury, soak the tooth in saline for 30 minutes followed by a doxycycline solution (1mg doxy in 20mL of saline) for 5 minutes prior to reimplantation and splinting to maximize the chances of revascularization and reintegration of the tooth.
Use teeth occlusion as a guide to positioning of the tooth during reimplantation.
Hold avulsed teeth by the crown of the tooth only; avoid handling the root of the tooth whenever possible to maintain the vitality of the periodontal ligament cells.
Pitfall: one pitfall in the management of an avulsed tooth is handling the root of the tooth; this may obfuscate tooth vitality. Always handle the tooth from the crown.
3 Dental splinting methods for dental avulsions and subluxations – wire method, periodontal paste method, N95 nose bridge method
Dental kit wire and composite dental splint method
Using the wires supplied in your ED dental kit, place wire across the tooth in question as well as the 2 adjacent teeth use the curing light to convert the liquid composite material into a solid material to adhere the wires to the teeth, as described in this video:
Periodontal paste dental splint method

Care of Core EM https://coreem.net/core/dental-trauma/
N95 mask metal nose bridge dental splint method
If a dental kit is not available in your ED, an N95 respiratory mask nose bridge with surgical skin glue is a recognized alternative. N95 mask metal nose bridge dental splint technique.

Care of ALiEM https://www.aliem.com/trick-of-trade-dental/
Indications for antibiotics in dental trauma, infection prevention after dental trauma with chlorhexidine
Antibiotics are generally not indicated for isolated dental avulsions or fractures, and should be reserved for open dental alveolar fractures, however chlorhexidine mouth washes twice daily for 7 days have been recommended to prevent infectious complications.
Management of complicated dental fractures with exposed pulp using calcium hydroxide
Do not attempt reimplantation of a complicated crown fracture, fractured root or dental injury with alveolar fracture.For complicated dental fractures involving exposed pulp (pink dot on exam), calcium hydroxide should be applied in the ED by mixing the catalyst and the base in an equal ratio, drying the surface of the tooth with gauze or air and applying a small amount to cover the exposed pulp. Follow up with a dentist is recommended for consideration of root canal.
Pearl: If calcium hydroxide is not available in your ED, surgical skin glue (eg. Dermabond, Swiftset) is a reasonable alternative for covering exposed pulp in a complicated dental fracture
Management of acute dental bleeding in the ED
First line: Soak gauze with tranexamic acid (500mg in 10mL) and apply pressure by instructing the patient bite down hard continuously for 30 minutes.
Second line: If the above method fails, consider injection of 2% xylocaine with epinephrine into the source of bleeding and the surrounding gingiva until blanching of the tissue is visible, followed by repeated pressure by biting down on gauze for the 30 minutes. The analgesia provided allows the patient to apply adequate pressure without causing pain.
Educating patients about post dental trauma risks
At ED discharge is important to set expectations about possible post dental trauma risks that include:
- Tooth resorption complications (progressive loss of part or parts of the tooth)
- Discoloration of tooth (dark tooth as a result of bleeding within the tooth)
- Pulp necrosis
- Loss of tooth
- Requirement for root canal procedure