פוסט זה זמין גם ב:
עברית
September 9, 2022 / Cardiology, Ultrasound
Written by Seth Walsh-Blackmore
Spoon Feed
This is an EM-focused review of pericardial tamponade, including the bedside echo.
Why does this matter?
Pericardial tamponade is rare and deadly, with a non-specific presentation in which early recognition can save a life.
Pericardial tamponade – What you need to know (Spoiler: It’s not Beck’s triad)
The Basics
- Five cases per 10,000 admissions
- Malignancy was the most common etiology (15-65% of cases). The next was idiopathic (4-37%).
- Dyspnea was the most consistent symptom at 66-90%. Other symptoms varied substantially.
- Most common exam finding was HR >100 (65-88%).
- Hypotension is not a reliable finding. SBP < 100 mmHg was only recorded in 14-35% of non-traumatic cases, and 27-43% had an SBP > 140 mmHg.
- No patient had all three elements of Beck’s Triad (hypotension, JVD, muffled heart sounds).
- Most common ECG finding was sinus tachycardia (47-88%). The classic electrical alternans was seen in 3-21%.
- POCUS is the first line modality for diagnosis. It reduced time to drainage in clinically significant effusions. Cardiologists agree.
How to echo
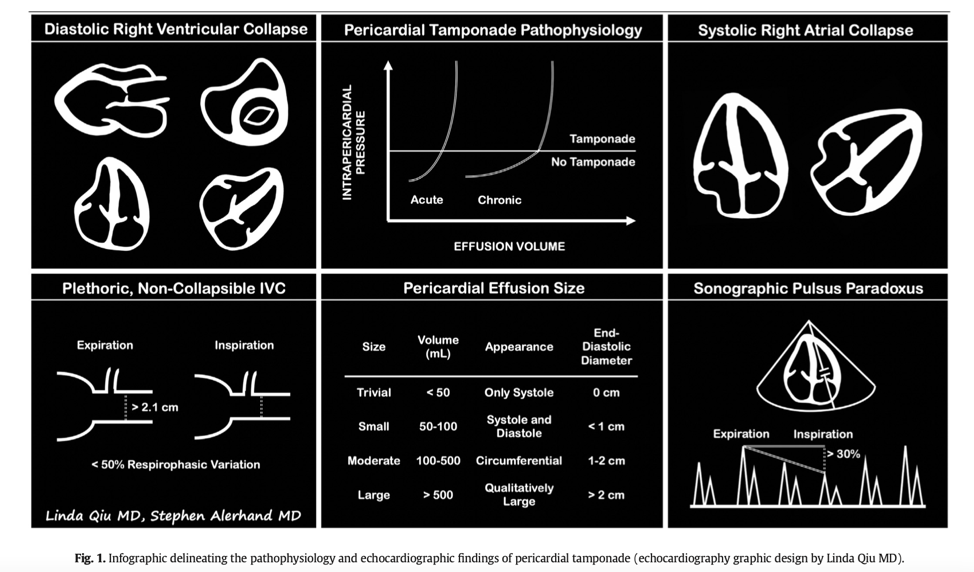
- Obtain multiple views to increase sensitivity for pericardial effusion. Size estimation: visible only in systole (<50ml), systole + diastole (50-100ml), appears circumferential (>100ml – more likely to be significant).
- An IVC >2.1cm with < 50% respiratory collapse was 95-97% sensitive (not specific) for tamponade. Visual estimation is fine in urgent situations.
- Right atrial systolic collapse is the earliest finding, with higher sensitivity for tamponade, and becomes more specific if duration is > 1/3 of the cardiac cycle. Need apical 4 chamber or subxiphoid view.
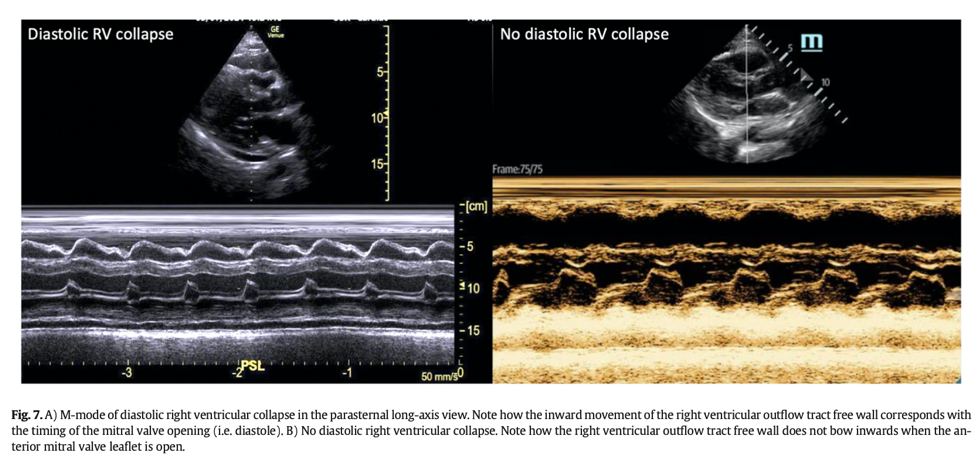
- Right ventricle free wall diastolic collapse is the more specific finding (75-90% specific; 48-60% sensitive). Any view works. Try parasternal long with M-mode through the RV outflow tract free wall and tip of anterior mitral leaflet, which allows you to properly identify when collapse is occurring in relation to the cardiac cycle.
- Lack of any right-sided chamber collapse has an NPV of 90% for most tamponade (but not from infectious or loculated effusion).
Management
- There is a scoring system for the urgency of drainage. The stable patient can wait for backup. In hemodynamic shock, it needs drainage now.
- Fluids/blood for volume depletion only. Start low (250-500ml).
- Consider inotropes that reduce SVR and induce tachycardia in an attempt to increase cardiac output (isoproterenol, low-dose epinephrine)
- Don’t aggressively treat hypertension. The BP will likely drop after drainage.
- Avoid positive pressure ventilation if you can. If you must, attempt drainage before, or at least delay until ready to drain.
Drainage Tips
- The best view is the one with the largest pocket, closest to the skin.
- It is easy to underestimate the distance from the skin to the effusion due to probe pressure on the soft tissue.
- The phased array probe is poor at needle guidance. Use curvilinear or linear and minimize depth to help with needle visualization.
- Elevating the head of the bead helps get fluid anterior and inferior.
- Injecting agitated saline is a method to confirm needle placement if uncertain.
- A small amount of drainage can stabilize hemodynamics, while draining a large effusion too fast can cause a decompression syndrome
Another Spoonful
- I highly recommend viewing the full article online for videos and more images. Jacob Avila, an author of this paper, has additional videos to learn the bedside echo on CORE Ultrasound.
- Other tips from an ultrasound pro, Megan Hilbert:
- Tamponade is a clinical diagnosis.
- While we estimate the size of the effusion, it is often the rate of accumulation that is more clinically significant than total volume.
- If quantitatively evaluating the size of an effusion – measure diameter between visceral and parietal pericardium at end-diastole.
- You can also calculate ultrasonographic pulsus paradoxus using pulsed wave Doppler to measure respiratory variation of mitral inflow velocities in the apical 4 view. With > 25% change in E-wave velocities representing tamponade physiology in spontaneously breathing patients.
Edited by Megan Hilbert
Source
Pericardial tamponade: A comprehensive emergency medicine and echocardiography review. Am J Emerg Med. 2022 Aug;58:159-174. doi: 10.1016/j.ajem.2022.05.001. Epub 2022 May 6.





