פוסט זה זמין גם ב:
עברית
Written by Bo Stubblefield
Spoon Feed
The European Society of Cardiology (ESC) has generated a position detailing optimal follow-up of patients following acute pulmonary embolism (PE). They advocate for a holistic approach with consideration of both short- and long-term events encountered by patients diagnosed with acute PE.
Why does this matter?
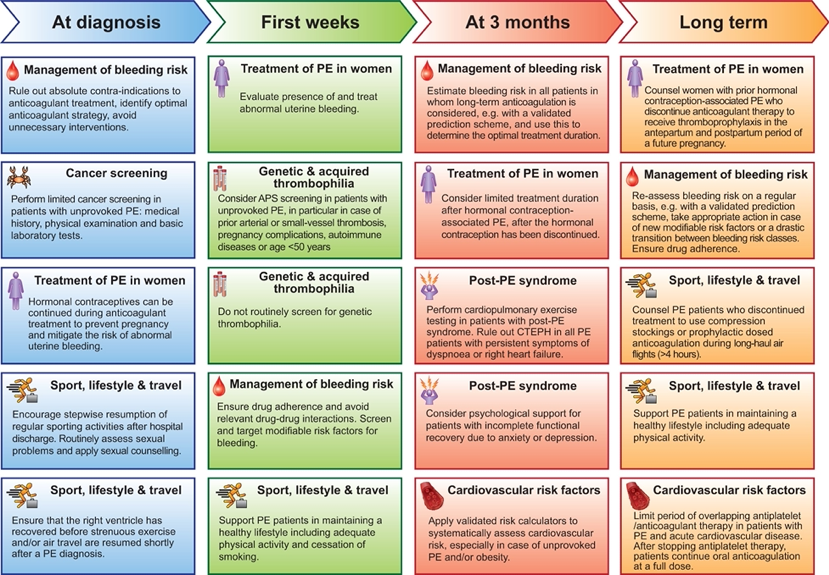
Patients with acute PE are a heterogenous population. They require individualized therapies both at presentation and during long-term follow up. This position paper complements the formal 2019 ESC Guidelines.1 Recommendations in this position paper include management of bleeding risk, treatment of PE in women, cancer and thrombophilia screening, sport, lifestyle, and travel considerations, assessment of cardiovascular risk factors, and management of post-PE syndrome.
PE? Check. Now what?
Here is a break-down of PE management considerations by timeline (Fig 1):
At Diagnosis:
- Rule out absolute contraindications to anticoagulation, optimize anticoagulation strategies, avoid unnecessary interventions .
- Only a limited (age-appropriate) screen for cancer is recommended.
First Weeks:
- Encourage patients to resume regular exercise in a stepwise manner
- Ensure the right ventricle has recovered in size and function before resuming exercise or air travel.
- Do not routinely screen for inherited thrombophilia.
- Consider anti-phospholipid antibody syndrome in patients with unprovoked PE.
- Ensure anticoagulant adherence.
- Continue to screen for modifiable risk factors for bleeding.
3 Months:
- Perform cardiopulmonary exercise testing (CPET) in patients with persistent dyspnea.
- Rule out chronic thromboembolic pulmonary hypertension (CTEPH).
- Consider psychological support.
- Systematically assess general cardiovascular risk factors.
Long Term:
- Limit periods of overlap between antiplatelet and anticoagulant medications in those taking anticoagulation beyond 3 months.
- As many as 40% of survivors have persistent dyspnea at 6-12 months2, and 30-50% have persistent functional limitations at 12-24 months.3,4
- The concept that PE causes persistent symptoms has been noted for decades, but only recently has investigation into the incidence and general mechanism begun. The combination of functional impairment and dyspnea is now called post-PE syndrome.5-8
Fig 1.
Another Spoonful
Geoff Barnes outlines 10 key points from this position paper on the American College of Cardiology Website.
Still hungry? One more Spoonful…
Check out these reviews to bulk up your knowledge on post-PE syndrome:
- Post-PE syndrome: a new concept for chronic complications of PE
- Late outcomes of PE: The post-PE syndrome
Source
Optimal follow-up after acute pulmonary embolism: a position paper of the European Society of Cardiology Working Group on Pulmonary Circulation and Right Ventricular Function, in collaboration with the European Society of Cardiology Working Group on Atherosclerosis and Vascular Biology, endorsed by the European Respiratory Society. Eur Heart J. 2022 Jan 25;43(3):183-189. doi: 10.1093/eurheartj/ehab816.





